Abstract
This article presents a systematic review of pharmacological treatment for negative symptoms of schizophrenia, based on MEDLINE searches from 1995 to September 2002 to identify pertinent clinical trials. The pharmacotherapy of negative symptoms in schizophrenia includes novel/atypical antipsychotics and classical antipsychotics, as well as antidepressants, glutamatergic compounds, antiepileptic drugs and estrogens. In the assessment of therapy for negative symptoms of schizophrenia, it is imperative that better studies of sound methodology are performed. In such studies, some important aspects to be considered include an accurate definition and assessment of negative symptoms (including well designed, valid and reliable rating scales), the differentiation between primary and secondary negative symptoms, an appropriate selection of standard comparators, adequate dosages of comparators (e.g. haloperidol dosages) and an overall optimal study design.
Most of the available studies on treating negative symptoms in schizophrenia have focused on the atypical antipsychotics, while other potential candidates, mostly in the context of add-on therapy, have not been so intensively investigated. Atypical antipsychotics have been proven in placebo-controlled trials to be effective in treating negative symptoms of acute schizophrenic episodes. In many of the comparator studies, they showed efficacy in treating negative symptoms that was superior to that of typical antipsychotics. Data on stable, predominant negative symptoms in subchronic or chronic cases of schizophrenia, although limited, have demonstrated the efficacy of atypical antipsychotics. If the beneficial tolerability profile with respect to extrapyramidal symptoms is also taken into account during clinical decision making, the atypical antipsychotics should be preferred for the treatment of negative symptoms. It is also worth noting that the traditional antipsychotics have the risk of inducing negative symptoms in the context of akinesia.
The benefits of add-on therapy with SSRIs or a glutamatergic compound are well documented. Estrogen add-on therapy seems promising. Other traditionally suggested approaches, such as comedication with an antiepileptic drug, lithium or β-adrenoceptor antagonist, cannot generally be recommended on the basis of the available data.





Similar content being viewed by others
References
Möller HJ. Atypical neuroleptics: a new approach in the treatmentof negative symptoms. Eur Arch Psychiatry Clin Neurosci1999; 249Suppl. 4: IV/99–107
Heinssen RK, Liberman RP, Kopelowicz A. Psychosocial skills training for schizophrenia: lessons from the laboratory. Schizophr Bull 2000; 26: 21–46
Treatment of schizophrenia 1999: the expert consensus guideline series. J Clin Psychiatry 1999; 60Suppl.11: 3–80
Lehman AF, Steinwachs DM. Translating research into practice:the schizophrenia Patient Outcomes Research Team(PORT) treatment recommendations. Schizophr Bull 1998; 24:1–10
Meltzer HY, Zureick J. Negative symptoms in schizophrenia: atarget for new drug development. In: Dahl SG, Gram LF, editors. Clinical pharmacology in psychiatry. Berlin: Springer,1989: 68–77
Rösier M, Hengesch G. Negative symptoms in the AMDPsystem [in German]. In: Baum U, Fähndrich E, Stieglitz RD, et al., editors. Measurement of changes in psychiatry and clinical psychology [in German]. München: Profil, 1990: 329–39
Crow TJ. The two-syndrome concept: origins and current status.Schizophr Bull 1985; 11: 471–86
Strauss JS, Carpenter Jr WT, Bartko JJ. The diagnosis andunderstanding of schizophrenia: part III. Speculations on the processes that underlie schizophrenic symptoms and signs. Schizophr Bull 1974; 11: 61–9
Wing JK. The concept of negative symptoms. Br J Psychiatry Suppl 1989; 7: 10–4
Overall J, Gorham D. Brief psychiatric rating scale. Psychol Rep 1962; 10: 799–812
Krawiecka M, Goldberg D, Vaughan M. A standardized psychiatric assessment scale for rating chronic psychotic patients. Acta Psychiatr Scand 1977; 55: 299–308
Crow TJ. Molecular pathology of schizophrenia: more than one disease process? BMJ 1980; 280: 66–8
Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 1987; 13: 261–76
Andreasen NC. Negative symptoms in schizophrenia: definition and reliability. Arch Gen Psychiatry 1982; 39: 784–8
Abrams R, Taylor MA. A rating scale for emotional blunting. Am J Psychiatry 1978; 135: 226–9
Maier W, Schlegel S, Klinger T, et al. Die negativsymptomatik im Verhältnis zur positivsymptomatik und zur depressivenSymptomatik der schizophrenie: eine psychometrische Untersuchung. In: Möller HJ, Pelzer E, editors. Neuere ansätze zur diagnostik und therapie schizophrener minussymptomatik. Berlin: Springer, 1990: 69–78
Möller HJ. Konsequenzen aus der klinischen psychopharmakologie für die nosologische und syndromatologische klassifikation funktioneller psychischer Störungen. In: Simhandl CH, Berner P, Luccioni H, et al., editors. Klassifikationsprobleme in der psychiatrie. Pukersdorf: Med.-pharmazeutische Verlagsgesellschaft, 1987: 163–88
Hoffman WF, Labs SM, Casey DE. Neuroleptic-induced parkinsonism in older schizophrenics. Biol Psychiatry 1987; 22: 427–39
Prosser ES, Csernansky JG, Kaplan J, et al. Depression, parkin-sonian symptoms, and negative symptoms in schizophrenics treated with neuroleptics. J Nerv Ment Dis 1987; 175: 100–5
Angst J, Stassen HH, Woggon B. Effect of neuroleptics on positive and negative symptoms and the deficit state. Psycho-pharmacology Berl 1989; 99 Suppl.: S41–6
Marneros A, Deister A, Rohde A. Affektive, schizoaffektiveund schizophrene psychosen: eine vergleichende langzeit-studie.Berlin: Springer, 1991
Carpenter WT Jr, Heinrichs DW, Alphs LD. Treatment of negative symptoms. Schizophr Bull 1985; 11: 440–52
Andreasen NC, Olsen S. Negative v positive schizophrenia: definition and validation. Arch Gen Psychiatry 1982; 39: 789–94
McGlashan TH, Fenton WS. The positive-negative distinction in schizophrenia: review of natural history validators. Arch Gen Psychiatry 1992; 49: 63–72
Möller HJ, Müller H, Borison RL, et al. A path-analytical approach to differentiate between direct and indirect drug effects on negative symptoms in schizophrenic patients: a re-evaluation of the North American risperidone study. Eur Arch Psychiatry Clin Neurosci 1995; 245: 45–9
Crow TJ. Positive and negative schizophrenic symptoms and the role of dopamine. Br J Psychiatry 1980; 137: 383–6
Rao ML, Möller HJ. Biochemical findings of negative symptoms in schizophrenia and their putative relevance to pharmacologic treatment: a review. Neuropsychobiology 1994; 30: 160–72
Meisenzahl EM, Frodl T, Zetzsche T, et al. Investigation of a possible diencephalic pathology in schizophrenia. Psychiatry Res 2002; 115: 127–35
Meltzer HY. The role of serotonin in antipsychotic drug action. Neuropsychopharmacology 1999; 21: 106S-15S
Möller HJ. Definition, psychopharmacological basis and clinical evaluation of novel/atypical neuroleptics: methodological issues and clinical consequences. World J Biol Psychiatry 2000; 1: 75–91
Braus DF, Ende G, Weber-Fahr W, et al. Antipsychotic drug effects on motor activation measured by functional magnetic resonance imaging in schizophrenic patients. Schizophr Res 1999; 39: 19–29
Sharma T, Kuman V. The influence of antipsychotic treatment on cortical activations in patients with schizophrenia using functional magnetic resonance imaging [abstract]. Eur Psychiatry 2002; 17 Suppl. 1: 23
Möller HJ. Neuroleptic treatment of negative symptoms in schizophrenic patients: efficacy problems and methodological difficulties. Eur Neuropsychopharmacol 1993; 3: 1–11
Meltzer HY. Dopamine and negative symptoms in schizophrenia: critique of the type I-II hypothesis. In: Alpert M, editor. Controversies in schizophrenia. New York: Guilford, 1985: 110–36
van Kammen DP, Hommer DW, Malas KL. Effect of pimozide on positive and negative symptoms in schizophrenic patients: are negative symptoms state dependent? Neuropsychobiology 1987; 18: 113–7
Marder SR, Meibach RC. Risperidone in the treatment of schizophrenia. Am J Psychiatry 1994; 151: 825–35
Möller HJ, van Praag HM, Aufdembrinke B, et al. Negative symptoms in schizophrenia: considerations for clinical trials: working group on negative symptoms in schizophrenia. Psychopharmacology 1994; 115: 221–8
Committee for Proprietary Medicinal Products (CPMP). Note for guidance on the clinical investigation of medicinal products in the treatment of schizophrenia. London: The European Agency for the Evaluation of Medicinal Products, 1998
Loo H, Poirier-Littre MF, Theron M, et al. Amisulpride versus placebo in the medium-term treatment of the negative symptoms of schizophrenia. Br J Psychiatry 1997; 170: 18–22
Peuskens J. Risperidone in the treatment of patients with chronic schizophrenia: a multi-national, multi-centre, double-blind, parallel-group study versus haloperidol: Risperidone Study Group. Br J Psychiatry 1995; 166: 712–26
Beasley Jr CM, Tollefson G, Tran P, et al. Olanzapine versus placebo and haloperidol: acute phase results of the North American double-blind olanzapine trial. Neuropsychopharmacology 1996; 14: 111–23
Tran P, Beasley C, Tollefson G, et al. Acute and long-term results of the dose ranging double-blind olanzapine trial. XXth Collegium Internationale Neuro-Psychopharmacologicum (CINP) Congress; 1996 Jun 23–27; Melbourne
Petit M, Raniwalla J, Tweed J, et al. A comparison of an atypical and typical antipsychotic, zotepine versus haloperidol in patients with acute exacerbation of schizophrenia: a parallel-group double-blind trial. Psychopharmacol Bull 1996; 32: 81–7
Möller HJ, Müller WE, Bandelow B. Neuroleptikatherapie: pharmakologische grundlagen, klinisches wissen und therapeutisches vorgehen. Stuttgart: Wissenschaftliche Verlagsgesellschaft, 2000
Zimbroff DL, Kane JM, Tamminga CA, et al. Controlled, dose-response study of sertindole and haloperidol in the treatment of schizophrenia. Am J Psychiatry 1997; 154: 782–91
Beasley Jr CM, Sanger T, Satterlee W, et al. Olanzapine versus placebo: results of a double-blind, fixed-dose olanzapine trial. Psychopharmacology (Berl) 1996; 124: 159–67
Kane JM, Honigfeld G, Singer J, et al. Clozapine for the treatment-resistant schizophrenic: a double-blind comparison versus chlorpromazine/benztropine. Arch Gen Psychiatry 1988; 48: 789–96
Klieser E, Lehmann E, Kinzler E, et al. Randomized, double-blind, controlled trial of risperidone versus clozapine in patients with chronic schizophrenia. J Clin Psychopharmacol 1995; 15: 45S-51S
Hoyberg OJ, Fensbo C, Remvig J, et al. Risperidone versus perphenazine in the treatment of chronic schizophrenic patients with acute exacerbations. Acta Psychiatr Scand 1993; 88: 395–402
Huttunen MO, Piepponen T, Rantanen H, et al. Risperidone versus zuclopenthixol in the treatment of acute schizophrenic episodes: a double-blind parallel-group trial. Acta Psychiatr Scand 1995; 91: 271–7
Cooper SJ, Raniwalla J, Welch C. A placebo-controlled comparison of zotepine versus chlorpromazine in patients with acute exacerbation of schizophrenia [abstract]. Eur Neuropsychopharmacol 1996; 6Suppl. 3: 148
Jallon P, Picard F. Double-blind comparison of olanzapine versus risperidone in the treatment of schizophrenia and other psychotic disorders. J Clin Psychopharmacol 1997; 17: 407–18
Conley RR, Mahmoud R. A randomized double-blind study of risperidone and olanzapine in the treatment of schizophrenia or schizoaffective disorder. Am J Psychiatry 2001; 158: 765–74
Fleurot O, Bech P, Turjanski S. Amisulpride versus risperidone in the treatment of acute schizophrenia. Biol Psychiatry 1997; 42 Suppl. 1: 194S
Schooler NR. Comments on article by Tran and colleagues, “Double-blind comparison of olanzapine versus risperidone in treatment of schizophrenia and other psychotic disorders”. J Clin Psychopharmacol 1998; 18: 174–6
Möller HJ. Amisulpride: efficacy in the management of chronic patients with predominant negative symptoms of schizophrenia. Eur Arch Psychiatry Clin Neurosci 2001; 251: 217–24
Möller HJ. Amisulpride: a review of its efficacy in schizophrenia. Acta Psychiatr Scand 2000; 101: 17–22
Mota NE, Lima MS, Soares BG. Amisulpride for schizophrenia. Available in The Cochrane Library [database on disk and CD ROM]. Updated quarterly. The Cochrane Collaboration; issue 2. Oxford: Oxford Update Software, 2002: CD001357
Goff DC, Coyle JT. The emerging role of glutamate in the pathophysiology and treatment of schizophrenia. Am J Psychiatry 2001; 158: 1367–77
Möller HJ, Boyer P, Fleurot O, et al. Improvement of acute exacerbations of schizophrenia with amisulpride: a comparison with haloperidol. Psychopharmacology 1997; 132: 396–401
Peuskens J, Bech P, Möller HJ, et al. Amisulpride versus risperidone in the treatment of acute exacerbations of schizophrenia. Psychiatry Res 1999; 88: 107–17
Boyer P, Lecrubier Y, Puech AJ, et al. Treatment of negative symptoms in schizophrenia with amisulpride. Br J Psychiatry 1995; 166: 68–72
Speller JC, Barnes TR, Curson DA, et al. One-year, low-dose neuroleptic study of in-patients with chronic schizophrenia characterised by persistent negative symptoms: amisulpride vs haloperidol. Br J Psychiatry 1997; 171: 564–8
Colonna L, Saleem P, Dondey-Nouvel L, et al. Long-term safety and efficacy of amisulpride in subchronic or chronic schizophrenia: Amisulpride Study Group. Int Clin Psychopharmacol 2000; 15: 13–22
Kane JM, Carson WH, Saha AR, et al. Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder. J Clin Psychiatry 2002; 63: 763–71
Yeung PP, Carson WH, Saha A, et al. Efficacy of aripiprazole, a novel antipsychotic, in schizophrenia and schizoaffective disorder: results of a placebo-controlled trial with risperidone [abstract no. P.2.040]. Eur Neuropsychopharmacol 2001 Oct; 11Suppl. 3: S259–60
Daniel DG, Saha AR, Ingenito G, et al. Aripiprazole, a novel antipsychotic: overview of a phase II study result [abstract no. P.01.242]. Int J Neuropsychopharmacol 2000 Jul; 3Suppl. 1: S157
Petrie JL, Saha AR, McEvoy JP, et al. Aripiprazole, a new typical antipsychotic: phase 2 clinical trial result [abstract no. P.2.114]. Eur Neuropsychopharmacol 1997 Sep; 7Suppl. 2: S227
Kujawa M, Saha AR, Ingenito GG, et al. Aripiprazole for long-term maintenance treatment of schizophrenia [abstract no. P.4.E.032]. Int J Neuropsychopharmacol 2002 Jun; 5Suppl. 1: S186–7
Kujawa M, Saha AR, Ingenito GG, et al. Aripiprazole for long-term maintenance treatment of schizophrenia [poster]. XXIII Collegium Internationale Neuro-Psychopharmacologium (CINP) Congress; 2002 Jun 23-27; Montreal
Carson WH, Pigott TA, Saha AR, et al. Aripiprazole vs.placebo in the treatment of chronic schizophrenia [abstract no. P.4.E.033]. Int J Neuropsychopharmacol 2002 Jun; 5Suppl. 1: S187
Carson WH, Pigott TA, Saha AR, et al. Aripiprazole vs. placebo in the treatment of stable, chronic schizophrenia [poster]. XXIII Collegium Internationale Neuro-Psychopharmacologium (CINP) Congress; 2002 Jun 23–27; Montreal
McGavin JK, Goa KL. Aripiprazole. CNS Drugs 2002; 16: 779–86
Wahlbeck K, Cheine M, Essali MA. Clozapine versus typical neuroleptic medication for schizophrenia. Available in TheCochrane Library [database on disk and CD ROM]. Updated quarterly. The Cochrane Collaboration; issue 2. Oxford: Oxford Update Software, 2002: CD000059
Tuunainen A, Wahlbeck K, Gilbody SM. Newer atypical anti-psychotic medication versus clozapine for schizophrenia. Available in The Cochrane Library [database on disk and CD ROM]. Updated quarterly. The Cochrane Collaboration; issue 2. Oxford: Oxford Update Software, 2000: CD000966
Lindenmayer JP, Grochowski S, Mabugat L. Clozapine effects on positive and negative symptoms: a six-month trial in treatment-refractory schizophrenics. J Clin Psychopharmacol 1994; 14: 201–4
Meltzer HY. Dimensions of outcome with clozapine. Br J Psychiatry Suppl 1992; 17: 46–53
Meltzer HY, Bastani B, Kwon KY, et al. A prospective study of clozapine in treatment-resistant schizophrenic patients: I. Preliminary report. Psychopharmacology (Berl) 1989; 99 Suppl.: S68–72
Breier A, Buchanan RW, Kirkpatrick B, et al. Effects of clozapine on positive and negative symptoms in outpatients with schizophrenia. Am J Psychiatry 1994; 151: 20–6
Volavka J, Czobor P, Sheitman B, et al. Clozapine, olanzapine, risperidone, and haloperidol in the treatment of patients with chronic schizophrenia and schizoaffective disorder. Am J Psychiatry 2002; 159: 255–62
Beasley Jr CM, Tollefson GD, Tran PV. Efficacy of olanzapine:an overview of pivotal clinical trials. J Clin Psychiatry 1997;58 Suppl. 10: 7–12
Tollefson GD, Beasley Jr CM, Tran PV, et al. Olanzapineversus haloperidol in the treatment of schizophrenia andschizoaffective and schizophreniform disorders: results of aninternational collaborative trial. Am J Psychiatry 1997; 154: 457–65
Nemeroff CB. Dosing the antipsychotic medication olanzapine. J Clin Psychiatry 1997; 58Suppl. 10: 45–9
Duggan L, Fenton M, Dardennes RM, et al. Olanzapine forschizophrenia. Available in The Cochrane Library [databaseon disk and CD ROM]. Updated quarterly. The Cochrane Collaboration; issue 2. Oxford: Oxford Update Software, 2000: CD001359
Beasley Jr CM, Hamilton SH, Crawford AM, et al. Olanzapineversus haloperidol: acute phase results of the internationaldouble-blind olanzapine trial. Eur Neuropsychopharmacol 1997; 7: 125–37
Hamilton SH, Revicki DA, Genduso LA, et al. Olanzapineversus placebo and haloperidol: quality of life and efficacyresults of the North American double-blind trial. Neuropsychopharmacology 1998; 18: 41–9
Tollefson GD, Sanger TM. Negative symptoms: a path analytic approach to a double-blind, placebo- and haloperidol-controlledclinical trial with olanzapine. Am J Psychiatry 1997; 154: 466–74
Borison RL, Arvanitis LA, Miller BG, et al. ICI 204,636, an atypical antipsychotic: efficacy and safety in a multicenter, placebo-controlled trial in patients with schizophrenia. J Clin Psychopharmacol 1996; 16: 158–69
Small JG, Hirsch SR, Arvanitis LA, et al. Quetiapine in patients with schizophrenia: a high- and low-dose double-blind comparison with placebo: Seroquel Study Group. Arch Gen Psychiatry 1997; 54: 549–57
Arvanitis LA, Miller BG. Multiple fixed doses of “Seroquel” (quetiapine) in patients with acute exacerbation of schizophrenia: a comparison with haloperidol and placebo: the Seroquel Trial 13 Study Group. Biol Psychiatry 1997; 42: 233–46
Peuskens J, Link CG. A comparison of quetiapine and chlorpromazine in the treatment of schizophrenia. Acta Psychiatr Scand 1997; 96: 265–73
Srisurapanont M, Disayavanish C, Taimkaew K. Quetiapine for schizophrenia. Available in The Cochrane Library [database on disk and CD ROM]. Updated quarterly. The Cochrane Collaboration; issue 2. Oxford: Oxford Update Software, 2000: CD000967
Kennedy E, Song F, Hunter R, et al. Risperidone versus typical antipsychotic medication for schizophrenia. Available in The Cochrane Library [database on disk and CD ROM]. Updated quarterly. The Cochrane Collaboration; issue 2. Oxford: Oxford Update Software, 2000: CD000440
Gilbody SM, Bagnall AM, Duggan L, et al. Risperidone versusother atypical antipsychotic medication for schizophrenia. Available in The Cochrane Library [database on disk and CD ROM]. Updated quarterly. The Cochrane Collaboration; issue 3. Oxford: Oxford Update Software, 2000: CD002306
Bondolfi G, Baumann P, Patris M, et al. A randomized double-blind trial of risperidone versus clozapine for treatment-resistant chronic schizophrenia [abstract]. Eur Neuropsychopharmacol 1995; 5(3): 349
Csernansky JG, Mahmoud R, Brenner R. A comparison ofrisperidone and haloperidol for the prevention of relapse inpatients with schizophrenia. N Engl J Med 2002; 346: 16–22
Lewis R, Bagnall A, Leitner M. Sertindole for schizophrenia.Available in The Cochrane Library [database on disk and CDROM]. Updated quarterly. The Cochrane Collaboration; issue 2. Oxford: Oxford Update Software, 2000: CD001715
Targum S, Zborowski J, Henry M, et al. Efficacy and safety of sertindole in two double-blind, placebo-controlled trials of schizophrenic patients [abstract]. Eur Neuropsychopharmacol 1995; 5(3): 348
Hale A, Van der Burght M, Friberg HH, et al. Dose-ranging study comparing 4 doses of sertindole and 1 dose of haloperidol in schizophrenic patients [abstract]. Eur Neuropsychopharmacol 1996; 6Suppl. 3: 61
Wehnert A, Mack R, Stilwell C, et al. Direct effect of sertindole on the primary negative symptoms of schizophrenia: a PATH analysis [poster]. The 6th World Congress of Biological Psychiatry; 1997 Jun 22–27; Nice
Bagnall A, Lewis RA, Leitner ML. Ziprasidone for schizophrenia and severe mental illness. Available in The Cochrane Library [database on disk and CD ROM]. Updated quarterly.The Cochrane Collaboration; issue 2. Oxford: Oxford Update Software, 2000: CD001945
Tandon R, Harrigan E, Zorn SH. Ziprasidone: a novel anti-psychotic with unique pharmacology and therapeutic potential. J Serotonin Res 1997; 4: 159–77
Davis R, Markham A. Ziprasidone. CNS Drugs 1997; 8(2): 153–9
Daniel DG, Zimbroff DL, Potkin SG, et al. Ziprasidone 80 mg/ day and 160 mg/day in the acute exacerbation of schizophreniaand schizoaffective disorder: a 6-week placebo-controlledtrial. Neuropsychopharmacology 1999; 20(5): 491–505
Keck P, Buffenstein A, Ferguson J, et al. Ziprasidone 40 and 120 mg/day in the acute exacerbation of schizophrenia and schizoaffective disorder: a 4-week placebo-controlled trial. Psychopharmacology (Berl) 1998; 140: 173–84
Arato M, O’Connor R, Meltzer HY. A 1-year, double-blind, placebo-controlled trial of ziprasidone 40, 80 and 160 mg/day in chronic schizophrenia: the Ziprasidone Extended Use in Schizophrenia (ZEUS) study. Int Clin Psychopharmacol 2002; 17: 207–15
Dieterle DM, Muller SF, Ackenheil M. Effectiveness and tolerance of zotepine in a double-blind comparison with perazine in schizophrenic patients. Fortschr Neurol Psychiatr 1991; 59 Suppl. 1: 18–22
Fleischhacker WW, Barnas C, Stuppack CH, et al. Zotepine vs haloperidol in paranoid schizophrenia: a double-blind trial. Psychopharmacol Bull 1989; 25: 97–100
Klieser E, Lehmann E, Tegeler J. Double-blind comparison of 3 × 75mg zotepine and 3 × 4mg haloperidol in acute schizophrenic patients. Fortschr Neurol Psychiatr 1991; 59Suppl. 1: 14–7
Müller-Spahn F, Dieterle D, Ackenheil M. Clinical effectiveness of zotepine in treatment of negative schizophrenic symptoms: results of an open and a double-blind controlled trial. Fortschr Neurol Psychiatr 1991; 59 Suppl. 1: 30–5
Fenton M, Morris S, De Silva P, et al. Zotepine for schizophrenia.Available in The Cochrane Library [database on diskand CD ROM]. Updated quarterly. The Cochrane Collaboration;issue 2. Oxford: Update Software, 2000, CD001948
Barnas C, Stuppack CH, Miller C, et al. Zotepine in the treatment of schizophrenic patients with prevailingly negativesymptoms: a double-blind trial vs haloperidol. Int Clin Psychopharmacol 1992; 7: 23–7
Cooper SJ, Butler A, Tweed J, et al. Zotepine in the preventionof recurrence: a randomised, double-blind, placebo-controlled study for chronic schizophrenia. Psychopharmacology(Berl) 2000; 150: 237–43
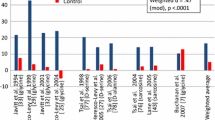
Leucht S, Pitschel-Walz G, Abraham D, et al. Efficacy and extrapyramidal side-effects of the new antipsychotics olanzapine, quetiapine, risperidone, and sertindole compared to conventional antipsychotics and placebo: a meta-analysis of randomized controlled trials. Schizophr Res 1999; 35: 51–68
Chakos M, Lieberman J, Hoffman E, et al. Effectiveness of second-generation antipsychotics in patients with treatment-resistant schizophrenia: a review and meta-analysis of randomized trials. Am J Psychiatry 2001; 158: 518–26
Geddes J, Freemantle N, Harrison P, et al. Atypical antipsychotics in the treatment of schizophrenia: systematic overview and meta-regression analysis. BMJ 2000; 321: 1371–6
Song F. Risperidone in the treatment of schizophrenia: a meta-analysis of randomized controlled trials. J Psychopharmacol 1997; 11: 65–71
Wahlbeck K, Cheine M, Essali A, et al. Evidence of clozapine’s effectiveness in schizophrenia: a systematic review and meta-analysis of randomized trials. Am J Psychiatry 1999; 156: 990–9
Leucht S, Pitschel-Walz G, Engel RR, et al. Amisulpride, an unusual “atypical” antipsychotic: a meta-analysis of randomized controlled trials. Am J Psychiatry 2002; 159: 180–90
Rosenthal R. Meta-analytic procedures for social research. 2nd ed. New York: Sage Publications, 1991
Conley RR, Tamminga CA, Bartko JJ, et al. Olanzapine compared with chlorpromazine in treatment-resistant schizophrenia. Am J Psychiatry 1998; 155: 914–20
Allan ER, Sison CE, Alpert M, et al. The relationship between negative symptoms of schizophrenia and extrapyramidal side effects with haloperidol and olanzapine. Psychopharmacol Bull 1998; 34: 71–4
Liu SK, Chen WJ, Chang CJ, etal. Effects of atypical neuroleptics on sustained attention deficits in schizophrenia: a trial of risperidone versus haloperidol. Neuropsychopharmacology 2000; 22: 311–9
Emsley RA. Risperidone in the treatment of first-episode psychotic patients: a double-blind multicenter study: Risperidone Working Group. Schizophr Bull 1999; 25: 721–9
See RE, Fido AA, Maurice M, et al. Risperidone-induced increase of plasma norepinephrine is not correlated with symptom improvement in chronic schizophrenia. Biol Psychiatry 1999; 45: 1653–6
Blin O, Azorin JM, Bouhours P. Antipsychotic and anxiolytic properties of risperidone, haloperidol, and methotrimeprazine in schizophrenic patients. J Clin Psychopharmacol 1996; 16: 38–44
Chouinard G, Jones B, Remington G, et al. A Canadian multi-center placebo-controlled study of fixed doses of risperidone and haloperidol in the treatment of chronic schizophrenic patients. J Clin Psychopharmacol 1993; 13: 25–40
Claus A, Bollen J, De Cuyper H, et al. Risperidone versus haloperidol in the treatment of chronic schizophrenic inpatients: a multicentre double-blind comparative study. Acta Psychiatr Scand 1992; 85: 295–305
Min SK, Rhee CS, Kim CE, et al. Risperidone versus haloperidol in the treatment of chronic schizophrenic patients: a parallel group double-blind comparative trial. Yonsei Med J 1993; 34: 179–90
Carman J, Peuskens J, Vangeneugden A. Risperidone in the treatment of negative symptoms of schizophrenia: a meta-analysis. Int Clin Psychopharmacol 1995; 10: 207–13
Danion JM, Rein W, Fleurot O. Improvement of schizophrenic patients with primary negative symptoms treated with amisulpride: Amisulpride Study Group. Am J Psychiatry 1999; 156: 610–6
Rüther E, Blanke J. Therapievergleich von aminosultoprid (DAN 2163) und perazin bei schizophrenen patienten. In: Helmchen H, Hippius H, Tölle R, editors. Therapie mit neuroleptika: perazin. Stuttgart: Georg Thieme Verlag, 1988: 65–71
Pichot P, Boyer P. Etude multicentrique controlée en double insu, amisulpride (Solian 200) versus halopéridol à forte dose dans les états psychotiques aigus. Ann Psychiatr 1988; 3: 326–32
Ziegler B. Study of the efficacy of a substituted benzamide amisulpride, versus haloperidol, in productive schizophrenia. In: Borenstein P, Boyer P, Braconnier A, et al., editors. Amisulpride. Paris: Expansion Scientifique Francaise, 1989: 73–82
Klein HE, Dieterle D, Rüther E, et al. A double-blind comparisonof amisulpride vs haloperidol in acute schizophrenic patients.In: Pichot P, Berner P, Wolf R, et al., editors. Psychiatry: the state of the art. Vol. 3. Pharmacopsychiatry. Cambridge (MA): Perseus Books, 1985: 687–91
Costa e Silva JA. Comparative double-blind study of amisulpride versus haloperidol in the treatment of acute psychotic states. In: Borenstein P, Boyer P, Braconnier A, et al., editors. Amisulpride. Paris: Expansion Scientifique Francaise, 1989: 93–104
Delcker A, Schoon ML, Oczkowski B, et al. Amisulpride versus haloperidol in treatment of schizophrenic patients: results of a double-blind study. Pharmacopsychiatry 1990; 23: 125–30
Wetzel H, Grander G, Hillert A, et al. Amisulpride versus flupentixol in schizophrenia with predominantly positive symptomatology: a double-blind controlled study comparing a selective D2-like antagonist to a mixed D1-/D2-like antagonist: the Amisulpride Study Group. Psychopharmacology (Berl) 1998; 137: 223–32
Puech A, Fleurot O, Rein W. Amisulpride, and atypical anti-psychotic, in the treatment of acute episodes of schizophrenia: a dose-ranging study vs haloperidol: the Amisulpride Study Group. Acta Psychiatr Scand 1998; 98: 65–72
Carriere P, Bonhomme D, Lemperiere T. Amisulpride has a superior benefit/risk profile to haloperidol in schizophrenia: results of a multicentre, double-blind study: the Amisulpride Study Group. Eur Psychiatry 2000; 15: 321–9
Paillere-Martinot ML, Lecrubier Y, Martinot JL, et al. Improvement of some schizophrenic deficit symptoms with low doses of amisulpride. Am J Psychiatry 1995; 152: 130–4
Pichot P, Boyer P. Controlled double-blind multi-centre trial of low dose amisulpride versus fluphenazine in the treatment of the negative syndrome of chronic schizophrenia. In: Borenstein P, Boyer P, Braconnier A, et al., editors. Amisulpride. Paris: Expansion Scientifique Francaise, 1989: 125–38
Saletu B, Kufferle B, Grunberger J, et al. Clinical, EEG mapping and psychometric studies in negative schizophrenia: comparative trials with amisulpride and fluphenazine. Neuropsychobiology 1994; 29: 125–35
Siris SG, Bermanzohn PC, Gonzalez A, et al. The use of antidepressants for negative symptoms in a subset of schizophrenic patients. Psychopharmacol Bull 1991; 27: 331–5
Silver H, Nassar A. Fluvoxamine improves negative symptoms in treated chronic schizophrenia: an add-on double-blind, placebo-controlled study. Biol Psychiatry 1992; 31: 698–704
Waehrens J, Gerlach J. Antidepressant drugs in anergic schizophrenia. Acta Psychiatr Scand 1980; 61: 438–44
Becker RE. Implications of the efficacy of thiothixene and achlorpromazine-imipramine combination for depression in schizophrenia. Am J Psychiatry 1983; 140: 208–11
Plasky P. Antidepressant usage in schizophrenia. Schizophr Bull 1991; 17: 649–57
Kramer M, Vogel W, DiJohnson C, et al. Antidepressants in “depressed” schizophrenic inpatients: a controlled trial. Gen Psychiatry 1989; 46: 922–8
Prusoff VA, Williams DH, Weissman MM, et al. Treatment of secondary depression in schizophrenia. Arch Gen Psychiatry 1979; 36: 569–75
Goff DC, Midha KK, Brotman A, et al. Elevation of plasma concentrations of haloperidol after addition of fluoxetine. AmJ Psychiatry 1991; 148: 790–2
Goff DC, Midha KK, Sarid-Segal O, et al. A placebo-controlled trial of fluoxetine added to neuroleptic in patients with schizophrenia. Psychopharmacology (Berl) 1995; 117: 417–23
Centorrino F, Baldessarini RJ, Kando J, et al. Serum concentrations of clozapine and its major metabolites: effects of cotreatment with fluoxetine or valproate. Am J Psychiatry 1994; 151: 123–5
Breier A. Serotonin, schizophrenia and antipsychotic drug action. Schizophr Res 1995; 14: 187–202
Kapur S, Remington G. Serotonin-dopamine interaction and its relevance to schizophrenia. Am J Psychiatry 1996; 153: 466–76
Gelders Y, Van den Bussche G, Reyntjens A. Serotonin S-2 receptor blockers in the treatment of chronic schizophrenia. Clin Neuropharmacol 1986; 9: 325–7
Leysen JE, Janssen PMF, Schotte A, et al. Interaction of antipsychotic drugs with neurotransmitter receptor sites in vitro and in vivo in relation to pharmacological an clinical effects: role of 5HT2 receptors. Psychopharmacology 1993; 112: S40–54
Reyntjens A, Hoppenbrouwers ML, Van den Bussche G. Thymostenic effects of ritanserin (R55667), a centrally active serotonin-S2 blocker. Drug Dev Res 1986; 8: 205–11
Backus LI, Sharp T, Grahame-Smith DG. Behavioral evidence for a functional interaction between central 5-HT2 and 5-HT1Areceptors. Br J Pharmacol 1990; 100: 793–9
Hashimoto T, Kitamura N, Kajimoto Y, et al. Differential changes in serotonin 5-HT1A and 5-HT2 receptor binding in patients with chronic schizophrenia. Psychopharmacology (Berl) 1993; 112: S35–9
Ugedo L, Grenhoff J, Svensson TH. Ritanserin, a 5-HT2 receptorantagonist, activates midbrain dopamine neurons by blockingserotonergic inhibition. Psychopharmacology 1989; 98:45–50
Silver H, Shmugliakov N. Augmentation with fluvoxamine butnot maprotiline improves negative symptoms in treated schizophrenia:evidence for a specific serotonergic effect from adouble-blind study. J Clin Psychiatry 1998; 18: 208–11
Goff DC, Brotman A, Waites M, et al. Trial of fluoxetine added to neuroleptics for treatment-resistant schizophrenic patients. Am J Psychiatry 1990; 147: 492–4
Goldman MB, Janecek HM. Adjunctive fluoxetine improvesglobal function in chronic schizophrenia. J Neuropsychiatr 1990; 2: 429–31
Spina E, De Domenico P, Ruello C, et al. Adjunctive fluoxetine in the treatment of negative symptoms in chronic schizophrenicpatients. Int Clin Psychopharmacol 1994; 9: 281–5
Buchanan RW, Kirkpatrick B, Bryant N, et al. Fluoxetineaugmentation of clozapine treatment in patients with schizophrenia.Am J Psychiatry 1996; 153: 1625–7
Arango C, Kirkpatrick B, Buchanan RW. Fluoxetine as an adjunct to conventional antipsychotic treatment of schizophrenia patients with residual symptoms. J Nerv Ment Dis 2000; 188: 50–3
Taiminen TJ, Syvalahti E, Saarijarvi S, et al. Citalopram as an adjuvant in schizophrenia: further evidence for a serotonergic dimension in schizophrenia. Int Clin Psychopharmacol 1997; 12: 31–5
Lee MS, Kim YK, Lee SK, et al. A double-blind study of adjunctive sertraline in haloperidol-stabilized patients with chronic schizophrenia. J Clin Psychopharmacol 1998; 18: 399–403
Berk M, Ichim C, Brook S. Efficacy of mirtazapine add on therapy to haloperidol in the treatment of the negative symptoms of schizophrenia: a double-blind randomized placebo-controlled study. Int Clin Psychopharmacol 2001; 16: 87–92
Berendsen HH, Broekkamp CL, Pinder RM. Mirtazapine enhances the effect of haloperidol on apomorphine-induced climbing behaviour in mice and attenuates haloperidol-induced catalepsy in rats. Psychopharmacology (Berl) 1998; 135: 284–9
Schutz G, Berk M. Reboxetine add on therapy to haloperidol in the treatment of schizophrenia: a preliminary double-blind randomized placebo-controlled study. Int Clin Psychopharmacol 2001; 16: 275–8
Tsai G, Passani LA, Slusher SB, et al. Abnormal excitatory neurotransmitter metabolism in schizophrenic brains. Arch Gen Psychiatry 1995; 52: 829–36
Cohen B, Rosenbaum G, Luby E, et al. Comparison of phencyclidine hydrochloride (sernyl) with other drugs: simulation of schizophrenic performance with phencyclidine hydrochloride (sernyl), lysergic acid diethylamide (LSD-25), and amobarbital (Amytal) sodium. II: symbolic and sequential thinking. Arch Gen Psychiatry 1962; 6: 79–85
Moller P, Husby R. The initial prodrome in schizophrenia: searching for naturalistic core dimensions of experience and behavior. Schizophr Bull 2000; 26: 217–32
Malhotra AK, Pinals DA, Weingartner H, et al. NMDA receptor function and human cognition: the effects of ketamine in healthy volunteers. Neuropsychopharmacology 1996; 14: 301–7
Newcomer JW, Farber NB, Jevtovic-Todorovic V, et al. Ketamine-induced NMDA receptor hypofunction as a model of memory impairment and psychosis. Neuropsychopharmacology 1999; 20: 106–18
Deutch AY, Tam SY, Freeman AS, et al. Mesolimbic and mesocortical dopamine activation induced by phencyclidine: contrasting pattern to striatal response. Eur J Pharmacol 1987; 134: 257–64
Bowers Jr MB, Bannon MJ, Hoffman Jr FJ. Activation of forebrain dopamine systems by phencyclidine and footshock stress: evidence for distinct mechanisms. Psychopharmacology (Berl) 1987; 93: 133–5
Verma A, Moghaddam B. NMDA receptor antagonists impair prefrontal cortex function as assessed via spatial delayed alternation performance in rats: modulation by dopamine. J Neurosci 1996; 16: 373–9
Javitt DC, Zylberman I, Zukin SR, et al. Amelioration of negative symptoms in schizophrenia by glycine. Am J Psychiatry 1994; 151: 1234–6
Heresco-Levy U, Javitt DC, Ermilov M, et al. Double-blind, placebo-controlled, crossover trial of glycine adjuvant therapy for treatment-resistant schizophrenia. Br J Psychiatry 1996; 169: 610–7
Heresco-Levy U, Javitt DC, Ermilov M, et al. Efficacy of highdose glycine in the treatment of enduring negative symptoms of schizophrenia. Arch Gen Psychiatry 1999; 56: 29–36
Tsai G, Coyle JT. Glutamatergic mechanisms in schizophrenia. Annu Rev Pharmacol Toxicol 2002; 42: 165–79
Carfagno ML, Hoskins LA, Pinto ME, et al. Indirect modulation of dopamine D2 receptors as potential pharmacotherapy for schizophrenia: II. Glutamate (ant)agonists. Ann Pharmacother 2000; 34: 788–97
Krystal JH, D’Souza DC, Petrakis IL, et al. NMDA agonistsand antagonists as probes of glutamatergic dysfunction andpharmacotherapies in neuropsychiatric disorders. Harv RevPsychiatry 1999; 7: 125–43
Goff DC, Tsai G, Levitt J, et al. A placebo-controlled trial of D-cycloserine added to conventional neuroleptics in patients withschizophrenia. Arch Gen Psychiatry 1999; 56: 21–7
van Berckel BN, Evenblij CN, van Loon BJ, et al. D-cycloserine increases positive symptoms in chronic schizophrenic patients when administered in addition to antipsychotics: a double-blind, parallel, placebo-controlled study. Neuropsychopharmacology 1999; 21: 203–10
Goff DC, Henderson DC, Evins AE, et al. A placebo-controlled crossover trial of D-cycloserine added to clozapine in patients with schizophrenia. Biol Psychiatry 1999; 45: 512–4
Tsai GE, Yang P, Chung LC, et al. D-serine added to clozapinefor the treatment of schizophrenia. Am J Psychiatry 1999; 156:1822–5
Heresco-Levy U, Ermilov M, Shimoni J, et al. Placebo-controlledtrial of D-cycloserine added to conventional neuroleptics,olanzapine, or risperidone in schizophrenia. Am J Psychiatry 2002; 159: 480–2
Heresco-Levy U, Javitt DC, Ermilov M, et al. Efficacy of highdoseglycine in the treatment of enduring negative symptomsof schizophrenia. Arch Gen Psychiatry 1999; 56: 29–36
Evins AE, Fitzgerald SM, Wine L, et al. Placebo-controlled trial of glycine added to clozapine in schizophrenia. Am JPsychiatry 2000; 157: 826–8
Potkin SG, Jin Y, Bunney BG, et al. Effect of clozapine andadjunctive high-dose glycine in treatment-resistant schizophrenia.Am J Psychiatry 1999; 156: 145–7
Noorbala AA, Akhondzadeh S, Davari-Ashtiani R, et al.Piracetam in the treatment of schizophrenia: implications forthe glutamate hypothesis of schizophrenia. J Clin Pharm Ther 1999; 24: 369–74
Kulkarni J, Riedel A, de Castella AR, et al. Estrogen: a potentialtreatment for schizophrenia. Schizophr Res 2001; 48: 137–44
Seeman MV, Lang M. The role of estrogens in schizophreniagender differences. Schizophr Bull 1990; 16: 185–94
Hafner H, Behrens S, De Vry J, et al. An animal model for theeffects of estradiol on dopamine-mediated behavior: implicationsfor sex differences in schizophrenia. Psychiatry Res 1991; 38: 125–34
Hafner H, Riecher-Rossler A, An-Der-Heiden W, et al. Generatingand testing a causal explanation of the gender differencein age at first onset of schizophrenia. Psychol Med 1993; 23:925–40
Seeman MV. The role of estrogen in schizophrenia. J PsychiatryNeurosci 1996; 21: 123–7
Endo M, Daiguji M, Asano Y, et al. Periodic psychosis recurringin association with menstrual cycle. J Clin Psychiatry 1978; 39: 456–66
Riecher-Rossler A, Hafner H, Dutsch-Strobel A, et al. Furtherevidence for a specific role of estradiol in schizophrenia? BiolPsychiatry 1994; 36: 492–4
Foreman MM, Porter JC. Effects of catechol estrogens andcatecholamines on hypothalamic and corpus striatal tyrosinehydroxylase activity. J Neurochem 1980; 34: 1175–83
Di Paolo T, Payet P, Labrie F. Effect of chronic estradiol andhaloperidol treatment on striatal dopamine receptors. Eur JPharmacol 1981; 73: 105–6
Sumner BE, Fink G. Testosterone as well as estrogen increasesserotonin2A receptor mRNA and binding site densities in themale rat brain. Brain Res Mol Brain Res 1998; 59: 205–14
Deutsch SI, Rosse RB, Schwartz BL, et al. A revised excitotoxichypothesis of schizophrenia: therapeutic implications. ClinNeuropharmacol 2001; 24: 43–9
Busatto GF, Pilowsky LS, Costa DC, et al. Correlation betweenreduced in vivo benzodiazepine receptor binding and severityof psychotic symptoms in schizophrenia. Am J Psychiatry 1997; 154: 56–63
DeLorenzo RJ. Calcium-calmodulin systems in psychopharmacologyand synaptic modulation. PsychopharmacolBull 1983; 19: 393–7
Feinberg SS, Kay SR, Elijovich LR, et al. Pimozide treatmentof the negative schizophrenic syndrome: an open trial. J ClinPsychiatry 1988; 49: 235–8
Gould RJ, Murphy KM, Reynolds IJ, et al. Antischizophrenicdrugs of the diphenylbutylpiperidine type act as calcium channelantagonists. Proc Natl Acad Sci U S A 1983; 80: 5122-5
Gold PW, Robertson GL, Ballenger JC, et al. Carbamazepine diminishes the sensitivity of the plasma arginine vasopressin response to osmotic stimulation. J Clin Endocrinol Metab 1983; 57: 952–7
Brambilla F, Bondiolotti GP, Magioni M, et al. Vasopressin therapy in chronic schizophrenia: effects on negative symptoms and memory. Neuropsychobiology 1988; 20: 113–9
Barros HM, Braz S, Leite JR. Effect of carbamazepine on dopamine release and reuptake in rat striatal slices. Epilepsia 1986; 27: 534–7
Nachshoni T, Levin Y, Levy A, et al. A double-blind trial of carbamazepine in negative symptom schizophrenia. Biol Psychiatry 1994; 35: 22–6
Dose M, Apelt S, Emrich HM. Carbamazepine as an adjunct of antipsychotic therapy. Psychiatry Res 1987; 22: 303–10
Leucht S, McGrath J, White P, et al. Carbamazepine augmentation for schizophrenia: how good is the evidence? J Clin Psychiatry 2002; 63: 218–24
Hesslinger B, Normann C, Langosch JM, et al. Effects of carbamazepine and valproate on haloperidol plasma levels and on psychopathologic outcome in schizophrenic patients. J Clin Psychopharmacol 1999; 19: 310–5
Drapalski AL, Rosse RB, Peebles RR, et al. Topiramate improves deficit symptoms in a patient with schizophrenia when added to a stable regimen of antipsychotic medication. Clin Neuropharmacol 2001; 24: 290–4
Hesslinger B, Normann C, Langosch JM, et al. Effects of carbamazepine and valproate on haloperidol plasma levels and on psychopathologic outcome in schizophrenic patients. J Clin Psychopharmacol 1999; 19: 310–5
Wassef AA, Dott SG, Harris A, et al. Randomized, placebo-controlled pilot study of divalproex sodium in the treatment of acute exacerbations of chronic schizophrenia. J Clin Psychopharmacol 2000; 20: 357–61
Cheine M, Ahonen J, Wahlbeck K. Beta-blocker supplementation of standard drug treatment for schizophrenia. Available in The Cochrane Library [database on disk and CD ROM]. Updated quarterly. The Cochrane Collaboration; issue 3. Oxford: Oxford Update Software, 2000: CD000234
Wahlbeck K, Cheine MV, Gilbody S, et al. Efficacy of beta-blocker supplementation for schizophrenia: a systematic review of randomized trials. Schizophr Res 2000; 41: 341–7
Terao T, Oga T, Nozaki S, et al. Lithium addition to neuroleptic treatment in chronic schizophrenia: a randomized, double-blind, placebo-controlled, cross-over study. Acta Psychiatr Scand 1995; 92: 220–4
Schexnayder LW, Hirschowitz J, Sautter FJ, et al. Predictors of response to lithium in patients with psychoses. Am J Psychiatry 1995; 152: 1511–3
Pryor SR. Is platelet release of 2-arachidonoyl-glycerol a mediator of cognitive deficits? An endocannabinoid theory of schizophrenia and arousal. Med Hypotheses 2000; 55: 494–501
Meltzer H, Young M, Metz J, et al. Extrapyramidal side effects and increased serum prolactin following fluoxetine, a new antidepressant. J Neural Transm 1979; 45: 165–75
Lock J, Gwirtsman H, Targ E. Possible adverse drug interactions between fluoxetine and other psychotropics. Clin Psychopharmacol 1990; 10: 383–4
Tate JL. Extrapyramidal symptoms in a patient taking haloperidol and fluoxetine. Am J Psychiatry 1989; 146: 399–400
Baldessarini R, Marsh E. Fluoxetine and side effects. Arch GenPsychiatry 1990; 47: 191-2
Acknowledgements
No funding was used to assist in the preparation of this manuscript. The author has no potential conflicts of interest directly relevant to the contents of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Möller, HJ. Management of the Negative Symptoms of Schizophrenia. CNS Drugs 17, 793–823 (2003). https://doi.org/10.2165/00023210-200317110-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00023210-200317110-00003