-
PDF
- Split View
-
Views
-
Cite
Cite
Christina Rørbye, Mogens Nørgaard, Lisbeth Nilas, Medical versus surgical abortion: comparing satisfaction and potential confounders in a partly randomized study, Human Reproduction, Volume 20, Issue 3, 1 March 2005, Pages 834–838, https://doi.org/10.1093/humrep/deh643
Close - Share Icon Share
Abstract
BACKGROUND: The aim of the study was to compare satisfaction with medical and surgical abortion and to identify potential confounders affecting satisfaction. METHODS: 1033 women with gestational age (GA) ≤63 days had either a medical (600 mg mifepristone followed by 1 mg gemeprost) or a surgical abortion (vacuum aspiration in general anaesthesia). The procedure was determined either by randomization (n=111) or by choice (n=922). Data on satisfaction, side effects and expectations were collected from questionnaires 2 and 8 weeks after termination. RESULTS: More women were very satisfied or satisfied after a surgical than a medical abortion both after choosing method (92% vs 82%, P<0.0001), and after randomization (94% vs 68%, P<0.001). Satisfaction was higher after choosing a medical procedure than after randomization to the same procedure; 82% and 68%, respectively, P<0.05. Satisfaction with the medical procedure was inversely correlated with GA and the intensity of pain, nausea, vomiting and dizziness, while satisfaction with the surgical procedure was unaffected by these side effects. Fewer women with a failed medical than a failed surgical abortion were satisfied (17% vs 62%), P<0.05. CONCLUSIONS: Satisfaction with both medical and surgical abortions is high, although higher with the surgical than the medical procedure, and higher after choosing method than after randomization.
Introduction
In parts of the world where termination of pregnancy is performed under unsafe conditions, the medical method of termination has promising effects on maternal morbidity and mortality. In most parts of the western world however, both medical and surgical abortions are performed in safe and efficacious settings associated with low risks of complications (Heisterberg and Kringelbach, 1987; Hakim-Elahi et al., 1990; UK Multicentre Study, 1997; Kahn et al., 2000; Zhou et al., 2002). In this part of the world, the introduction of the medical abortion procedure is not a matter of saving lives, but rather a privilege of preference for one of two procedures.
When comparing medical and surgical abortion, focus should therefore not only be on efficacy and complications, but also on acceptability and patient satisfaction. Satisfaction with the medical abortion procedure is generally high (Beckman and Harvey, 1997; Winikoff et al., 1998; Honkanen and von Hertzen, 2002; Abdel-Aziz, 2004), but only few studies have compared satisfaction with the two methods. On this background we wanted to compare satisfaction with medical and surgical abortion performed in the same organization by the same personnel. Furthermore, we investigated if satisfaction is influenced by primary success, side effects, expectations and prior experiences.
Materials and methods
Women with gestational age (GA) ≤63 days (confirmed by trans-vaginal ultrasonography) when referred to Copenhagen Hospital H:S; Hvidovre and Frederiksberg for early termination of pregnancy in the period of August 2000 to June 2001, were assessed for eligibility to the study. Exclusion criteria were: less than 18 years of age, GA >63 days, insufficient language skills, asthma bronchiale requiring daily medication, lactation, suspicion of ectopic pregnancy or spontaneous abortion, coagulation disorder, multiple gestation and impairment of liver or kidney function. Efficacy was the primary outcome of the study while complications, side effects and acceptability were secondary outcomes.
Of 1135 eligible women 102 were either not addressed or did not want to participate in the study. The remaining 1033 were informed and counselled about the medical and the surgical abortion methods, about the design of the study, and signed an informed consent. All women were given the same written information about the two methods of termination supplemented with standardized oral information by a doctor on the pros and cons of the two methods without a recommendation of one method over the other. With the introduction of the medical method, the consultations were scheduled with an extra 10 min for questions and discussion about the two procedures. The women having a medical termination were told to expect pain like severe menstrual cramps during the expulsion and diminishing vaginal bleeding during the following 2 weeks. The women were offered randomization (through a centrally located telephone procedure) to either a medical or a surgical termination. If randomization was declined, the women chose method of termination. One hundred and eleven (11%) accepted randomization and 922 chose the method of termination. In the latter group, 332 (36%) chose a medical and 590 (64%) a surgical procedure. The study population has been described in detail earlier (Rorbye et al., 2004).
All women were screened for Chlamydia trachomatis in the cervix and the urethra, and if found positive treated with azithromycin 1 g prior to the abortion. The medical regimen was mifepristone 600 mg on day 1 followed by vagitorium gemeprost 1 mg on day 3. Pain and nausea were treated with morphine/metoclopramid supplemented with paracetamol/codeine by an hourly evaluation. The women were accompanied by a relative/friend as preferred, and one nurse treated three to four women in a standard hospital room. The women were informed to lie down in their bed 30 min after gemeprost administration, but were otherwise not restricted. They were discharged after 4–6 h, when the clinical situation allowed it. The surgical regimen was vacuum aspiration in general anaesthesia followed by a peroperative abdominal ultrasonography to ensure that the uterus was empty. Supplementary paracetamol 1 g was given post-operatively, and the women were discharged the same day. For priming, primi-gravidae were pre-treated with oral misoprostol 0.4 mg 8 h prior to surgery. After both procedures, the women were advised not to be alone until next morning (all the women lived within 10 min by car).
The women were asked to return for a follow-up visit 2 weeks later that included a clinical examination, and vaginal ultrasonography for women who had a medical abortion. At the follow-up visit the women filled out a questionnaire. Another questionnaire was mailed to both groups 8 weeks after the abortion. Data on baseline characteristics were obtained from the hospital records. Data on satisfaction, choice of method in the future, side effects, satisfaction with the counselling and expectations were obtained from the questionnaires. Satisfaction was categorized as very satisfied, satisfied, neither/nor, dissatisfied or very dissatisfied. The intensity of side effects were categorized as none, mild, moderate or severe. Prior to the study, 10 abortion-seeking women pre-tested both questionnaires.
Failure after both procedures was defined as subsequent surgical intervention or change of method within 3 months. The latter group included attempted surgical abortions, that were stopped because of mechanical difficulties (e.g. bicorn uterus) and followed by medical treatment, and medical abortions that were followed by a surgical intervention within a few hours after administration of gemeprost because of e.g. pain or severe bleeding. Using a unique personal identification code in a national computer system, there was no loss to follow-up in the analysis of efficacy. The local Ethical committee approved the study.
The groups were compared with Mann–Whitney U-test or Fischer's exact test.
Results
Among 2157 women referred to termination of pregnancy, 1135 were eligible for the study and 1033 accepted inclusion. Baseline characteristics were similar in women accepting and declining study participation, and in the two randomized groups. The randomized women had more prior induced abortions and were less educated than choosing women (Table I). Women who chose a medical termination differed slightly on age and GA, and differed on smoking habits and length of education (Table I). The response rate on the 2 week questionnaire was 81% (832/1033) and on both questionnaires 73% (751/1033). More non-responders were parous, more had prior spontaneous abortions, more were smokers and more were less educated than responders. Other baseline characteristics were similar.
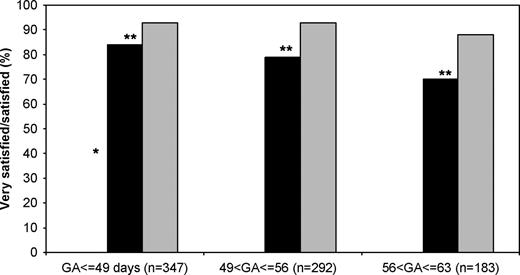
Two weeks after the abortion, more women were very satisfied or satisfied with a surgical than a medical procedure; 92% (95%CI: 90–94) and 79% (95%CI: 75–83) respectively, P<0.0001. This difference was larger among the randomized women; 94% and 68%, respectively, P<0.001 than among the choosing women; 92% and 82%, respectively, P<0.0001. The satisfaction with the medical procedure was higher after choosing than after randomization; 82% (95%CI: 78–86) vs 68% (95%CI: 55–81), P<0.05. Similar tendencies were found 8 weeks after the terminations. The lower level of satisfaction with the medical procedure was significant for all GAs (Figure 1). The satisfaction with the medical abortion procedure decreased with increasing GA, but was unrelated to GA after the surgical procedure (Figure 1). The satisfaction with the two methods was independent of age and parity, but a history of prior surgical termination was associated with fewer satisfied women after medical abortion (67%) compared to those with no prior abortions (87%), P<0.0001.
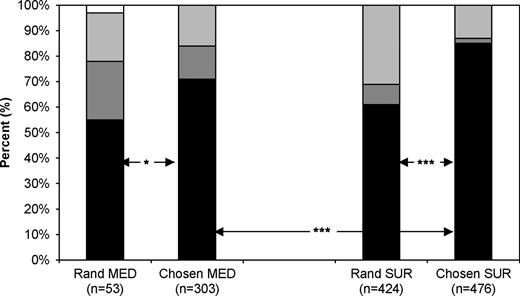
In case of a new unwanted pregnancy, more women would choose the same method again after a surgical than a medical abortion (82% vs 68%, P<0.0001) and more women would opt for the same method again if they had chosen the method rather being randomized (79% vs 58%, P<0.0001). Frequencies in each of the four groups are presented in Figure 2. The same trend was shown in method of recommendation to a friend, but with an even weaker loyalty toward the experienced method of termination.
Among women who had a former surgical abortion and now a medical, 46% (65/140) would in the future opt for a medical, 19% (27/140) for a surgical and 35% either did not know or did not answer the question. Twelve women had earlier experienced both a medical and a surgical abortion. Six of these now chose a medical, five a surgical and one was randomized.
The satisfaction with the counselling was high after both methods of termination. However, slightly more women were very satisfied/satisfied with the written information after a surgical than a medical termination (93% vs 89%, P<0.05), while satisfaction with the oral information was similar after both methods (96% vs 92%). Despite this evaluation, the abortion procedure experience was worse than expected by 27% of women choosing a medical and by 7% choosing a surgical termination, P<0.0001, and insignificantly worse after randomization than after choosing a medical procedure; 36% and 27%, respectively.
The overall success rate was lower after medical than after surgical abortion; 94.1% (386/410) vs 97.7% (708/725), P<0.01. Fewer were very satisfied/satisfied with a failed medical than a failed surgical procedure; 17% (3/18) respectively 62% (8/13), P<0.05.
The frequency of severe side effects was higher in women having a medical than a surgical abortion (Table II). Women experiencing severe side effects were less frequently satisfied with the medical procedure than women with less or no side effects (Table III). The same tendency was found among women with or without severe pain in relation to a surgical abortion (P=0.06), while no association was found between the other side effects and satisfaction with the surgical procedure. All side effects including intensity and duration of bleeding were unaffected by GA after both medical and surgical procedures. Women with a history of menstrual pain experienced severe pain more often than women without menstrual pain in relation to both a medical termination (57% vs 39%, P<0.05) and a surgical termination (19% vs 4%, P<0.0001). More nulliparous than parous women had severe pain in relation to both medical (56% vs 19%, P<0.0001) and surgical terminations (8% vs 3%, P<0.05).
At the 2 week follow-up, more women who had a medical than a surgical termination were still bleeding; 75% and 37%, respectively (P<0.0001). Among these, 24% and 11% characterized their bleeding as severe after a medical and a surgical procedure, respectively (P<0.0001).
Discussion
Several studies find that medical abortion is associated with high acceptability (Beckman and Harvey, 1997; Winikoff et al., 1998; Honkanen and von Hertzen, 2002; Abdel-Aziz, 2004). This is confirmed in the present study, but acceptability with the surgical procedure is even higher. The women randomized to a medical termination are furthermore less satisfied than those choosing the same method. Similar differences in patient satisfaction are found in earlier studies (Henshaw et al., 1993; Slade et al., 1998), and are found to persist in a 2 year follow-up trial (Howie et al., 1997). The quality of life is similarly improved after both methods (Westhoff et al., 2003). We also found that more women having a surgical than a medical procedure would opt for the same method again, which corresponds to earlier studies (Slade et al., 1998). In general though, patient satisfaction is complex and difficult to measure. To some extent it might be more a matter of culture, personal attitudes and general coping strategies than true satisfaction with a specific procedure.
The lower satisfaction with the medical procedure can be somewhat explained by the severe side effects. Although a single study showed no decrease in efficacy using nonsteroidal anti-inflammatory drugs (NSAID) as analgesic (Creinin and Shulman, 1997), NSAID was avoided in the present study to ensure no interaction between antiprostaglandin and gemeprost. Pain control is otherwise only described in relation to a methotrexate/misoprostol regimen, showing no difference in pain after randomization to placebo, ibuprofen or acetaminophen with codeine (Wiebe, 2001). It is possible that NSAID is preferable to morphine with a positive impact on satisfaction, but this is not addressed in the literature. Experience of pain in relation to a medical abortion may also be associated to psychological or social factors as seen in relation to surgical abortions in local anaesthesia (Belanger et al., 1989).
Counselling and expectations are other aspects with impact on satisfaction. As the counselling and the treatment was standardized and performed by the same personnel, the conditions for an acceptability study were optimized. In daily clinical practice however, it is impossible to eliminate the interpersonal variations of different doctors, or even different women's different interpretation of the same doctor's counselling (Bachelot et al., 1992; Lofgren, 2000). The satisfaction with both the written and oral information was high. The quality of the information in this study was probably higher than the generally inadequate information of poor readability found in a UK study (Wong et al., 2003). Despite this, more women having a medical than a surgical procedure found the procedure worse than expected, which might be explained by an overall minor experience with the new medical procedure or a difference in general coping strategies between women choosing the two methods.
During the study period, our medical abortion regimen consisted of mifepristone followed by gemeprost. Vaginally administered misoprostol has later replaced gemeprost due to lower costs and a potentially increased efficacy (Bartley et al., 2001). The side effects however seem similar, and the impact of choice of prostaglandin on satisfaction is probably minor.
Failure after a medical procedure is experienced as worse than failure after a surgical procedure, which might be explained by the later diagnosing of failed medical than failed surgical procedures (Rorbye et al., 2003), and the fact that a major reason for choosing a medical termination is to avoid a surgical procedure (Winikoff et al., 1998; Harvey et al., 2001; Honkanen and von Hertzen, 2002).
Women who choose medical and surgical abortions differ on socio-demographic variables (Bachelot et al., 1992; Cameron et al., 1996). They do not seem to differ on emotional status (Slade et al., 1998) or doubt about the abortion decision (Harvey et al., 2001), but might differ on other matters associated with satisfaction. The reason for randomization is avoiding these potential biases, including a probable loyalty toward a self-chosen method. As found in the present study, randomized and non-randomized patients also differ, which compromises the external validity of randomized studies (Olschewski et al., 1992; Dahler-Eriksen, 1998; Yuasa et al., 2003). Differences in emotional status and coping strategies may also be present, although this was not found in the Henshaw study (Henshaw et al., 1993). However, more than half of the women accepted randomization in the study of Henshaw, which might explain the similar baseline characteristics. Including both randomized and non-randomized women minimizes bias without the loss of external validity.
The abortion-seeking population includes women dedicated for both the medical and the surgical procedure (Gibb et al., 1998). The lower level of satisfaction in the randomized groups indicates that a choice between two methods is important for patient satisfaction. In our setting, satisfaction with both procedures was high, although more women were satisfied with the surgical than the medical procedure. While the choice between procedures has a positive influence on satisfaction, severe side effects and increasing GA have a negative influence. A medical regimen with fewer side effects, performed at an earlier limit for GA—perhaps in the privacy of the woman's home—might increase satisfaction with the medical procedure.
Satisfaction 2 weeks after medical (black boxes) and surgical abortions (grey boxes) stratified according to gestational age (GA). *P<0.05 between satisfaction with the medical procedure at different GA. Fischer's exact test. **P<0.01 between satisfaction with the medical and the surgical abortion procedure at three different GA.
Choice of future abortion procedure in the event of a new unwanted pregnancy. Black indicates choosing the same method as in this study. Dark grey indicates choosing ‘the other method’. Light grey indicates, ‘do not know’. White indicates no answer. *P<0.05 between women randomized and women choosing the medical (MED) procedure. ***P<0.001 between women choosing the medical and women choosing the surgical (SUR) procedure.
Baseline characteristics for randomized and choosing women and for women who chose a medical or a surgical termination
| . | Randomized to method (n=111) . | Chose method (n=922) . | Chose medical (n=332) . | Chose surgical (n=590) . |
|---|---|---|---|---|
| Age, median (range) | 26 (18–44) | 27 (18–45) | 28 (18–45)* | 27 (18–44) |
| GA, median (range) | 49 (22–60) | 51 (34–63) | 50 (33–63)** | 52 (35–63) |
| Prior induced abortion | 49%* | 38% | 35% | 40% |
| Prior spontaneous abortion | 14% | 15% | 14% | 15% |
| Multi-parity | 44% | 43% | 42% | 44% |
| BMI, median (range) | 23 (18–37) | 22 (13–43) | 22 (13–43) | 22 (16–43) |
| Smokers | 48% | 49% | 43%* | 52% |
| Educated >9 years | 46%** | 68% | 73%* | 65% |
| Married/living together | 36% | 43% | 44% | 42% |
| Employed/under education | 86% | 91% | 91% | 90% |
| . | Randomized to method (n=111) . | Chose method (n=922) . | Chose medical (n=332) . | Chose surgical (n=590) . |
|---|---|---|---|---|
| Age, median (range) | 26 (18–44) | 27 (18–45) | 28 (18–45)* | 27 (18–44) |
| GA, median (range) | 49 (22–60) | 51 (34–63) | 50 (33–63)** | 52 (35–63) |
| Prior induced abortion | 49%* | 38% | 35% | 40% |
| Prior spontaneous abortion | 14% | 15% | 14% | 15% |
| Multi-parity | 44% | 43% | 42% | 44% |
| BMI, median (range) | 23 (18–37) | 22 (13–43) | 22 (13–43) | 22 (16–43) |
| Smokers | 48% | 49% | 43%* | 52% |
| Educated >9 years | 46%** | 68% | 73%* | 65% |
| Married/living together | 36% | 43% | 44% | 42% |
| Employed/under education | 86% | 91% | 91% | 90% |
P<0.05.
P<0.01 (compared by Mann–Whitney and Fischer's exact test when appropriate) for randomized versus chose method and medical versus surgical.
GA, gestational age; BMI, body mass index.
Baseline characteristics for randomized and choosing women and for women who chose a medical or a surgical termination
| . | Randomized to method (n=111) . | Chose method (n=922) . | Chose medical (n=332) . | Chose surgical (n=590) . |
|---|---|---|---|---|
| Age, median (range) | 26 (18–44) | 27 (18–45) | 28 (18–45)* | 27 (18–44) |
| GA, median (range) | 49 (22–60) | 51 (34–63) | 50 (33–63)** | 52 (35–63) |
| Prior induced abortion | 49%* | 38% | 35% | 40% |
| Prior spontaneous abortion | 14% | 15% | 14% | 15% |
| Multi-parity | 44% | 43% | 42% | 44% |
| BMI, median (range) | 23 (18–37) | 22 (13–43) | 22 (13–43) | 22 (16–43) |
| Smokers | 48% | 49% | 43%* | 52% |
| Educated >9 years | 46%** | 68% | 73%* | 65% |
| Married/living together | 36% | 43% | 44% | 42% |
| Employed/under education | 86% | 91% | 91% | 90% |
| . | Randomized to method (n=111) . | Chose method (n=922) . | Chose medical (n=332) . | Chose surgical (n=590) . |
|---|---|---|---|---|
| Age, median (range) | 26 (18–44) | 27 (18–45) | 28 (18–45)* | 27 (18–44) |
| GA, median (range) | 49 (22–60) | 51 (34–63) | 50 (33–63)** | 52 (35–63) |
| Prior induced abortion | 49%* | 38% | 35% | 40% |
| Prior spontaneous abortion | 14% | 15% | 14% | 15% |
| Multi-parity | 44% | 43% | 42% | 44% |
| BMI, median (range) | 23 (18–37) | 22 (13–43) | 22 (13–43) | 22 (16–43) |
| Smokers | 48% | 49% | 43%* | 52% |
| Educated >9 years | 46%** | 68% | 73%* | 65% |
| Married/living together | 36% | 43% | 44% | 42% |
| Employed/under education | 86% | 91% | 91% | 90% |
P<0.05.
P<0.01 (compared by Mann–Whitney and Fischer's exact test when appropriate) for randomized versus chose method and medical versus surgical.
GA, gestational age; BMI, body mass index.
Frequency of severe side effects according to abortion method (medical or surgical) and to randomization (RAND) or choice of method
| . | Medical abortion . | . | . | Surgical abortion . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | Random (n=53) . | Chosen (n=303) . | Total (n=356) . | Random (n=52) . | Chosen (n=424) . | Total (n=476) . | ||||
| Severe pain | 42% | 40% | ***40% | 6% | 6% | 6% | ||||
| Severe bleeding | 35% | 36% | ***36% | 2% | 1% | 1% | ||||
| Severe nausea | 33% | 23% | ***25% | 15% | 10% | 11% | ||||
| Severe vomiting | 22% | 11% | ***13% | 2% | 1% | 2% | ||||
| Severe diarrhoea | 4% | 4% | ***4% | 2% | 0 | 0 | ||||
| Severe dizziness | 20% | 14% | ***15% | 4% | 1% | 2% | ||||
| . | Medical abortion . | . | . | Surgical abortion . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | Random (n=53) . | Chosen (n=303) . | Total (n=356) . | Random (n=52) . | Chosen (n=424) . | Total (n=476) . | ||||
| Severe pain | 42% | 40% | ***40% | 6% | 6% | 6% | ||||
| Severe bleeding | 35% | 36% | ***36% | 2% | 1% | 1% | ||||
| Severe nausea | 33% | 23% | ***25% | 15% | 10% | 11% | ||||
| Severe vomiting | 22% | 11% | ***13% | 2% | 1% | 2% | ||||
| Severe diarrhoea | 4% | 4% | ***4% | 2% | 0 | 0 | ||||
| Severe dizziness | 20% | 14% | ***15% | 4% | 1% | 2% | ||||
P<0.0001 compared to total surgical abortions, Fischer's exact test.
Frequency of severe side effects according to abortion method (medical or surgical) and to randomization (RAND) or choice of method
| . | Medical abortion . | . | . | Surgical abortion . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | Random (n=53) . | Chosen (n=303) . | Total (n=356) . | Random (n=52) . | Chosen (n=424) . | Total (n=476) . | ||||
| Severe pain | 42% | 40% | ***40% | 6% | 6% | 6% | ||||
| Severe bleeding | 35% | 36% | ***36% | 2% | 1% | 1% | ||||
| Severe nausea | 33% | 23% | ***25% | 15% | 10% | 11% | ||||
| Severe vomiting | 22% | 11% | ***13% | 2% | 1% | 2% | ||||
| Severe diarrhoea | 4% | 4% | ***4% | 2% | 0 | 0 | ||||
| Severe dizziness | 20% | 14% | ***15% | 4% | 1% | 2% | ||||
| . | Medical abortion . | . | . | Surgical abortion . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | Random (n=53) . | Chosen (n=303) . | Total (n=356) . | Random (n=52) . | Chosen (n=424) . | Total (n=476) . | ||||
| Severe pain | 42% | 40% | ***40% | 6% | 6% | 6% | ||||
| Severe bleeding | 35% | 36% | ***36% | 2% | 1% | 1% | ||||
| Severe nausea | 33% | 23% | ***25% | 15% | 10% | 11% | ||||
| Severe vomiting | 22% | 11% | ***13% | 2% | 1% | 2% | ||||
| Severe diarrhoea | 4% | 4% | ***4% | 2% | 0 | 0 | ||||
| Severe dizziness | 20% | 14% | ***15% | 4% | 1% | 2% | ||||
P<0.0001 compared to total surgical abortions, Fischer's exact test.
Frequency of women stating that they were very satisfied or satisfied with the medical abortion procedure according to the intensity of side effects (n=356)
| . | Severe side effects . | None, mild or moderate side effects . |
|---|---|---|
| Pain | 72%*** | 87% |
| Bleeding | 78% | 83% |
| Nausea | 68%** | 85% |
| Vomiting | 67%* | 83% |
| Diarrhoea | 62% | 83% |
| Dizziness | 65%** | 84% |
| . | Severe side effects . | None, mild or moderate side effects . |
|---|---|---|
| Pain | 72%*** | 87% |
| Bleeding | 78% | 83% |
| Nausea | 68%** | 85% |
| Vomiting | 67%* | 83% |
| Diarrhoea | 62% | 83% |
| Dizziness | 65%** | 84% |
P<0.05.
P<0.01.
P<0.001 comparing the frequency of satisfied women according to the presence of severe side effects, Fischer's exact test.
Frequency of women stating that they were very satisfied or satisfied with the medical abortion procedure according to the intensity of side effects (n=356)
| . | Severe side effects . | None, mild or moderate side effects . |
|---|---|---|
| Pain | 72%*** | 87% |
| Bleeding | 78% | 83% |
| Nausea | 68%** | 85% |
| Vomiting | 67%* | 83% |
| Diarrhoea | 62% | 83% |
| Dizziness | 65%** | 84% |
| . | Severe side effects . | None, mild or moderate side effects . |
|---|---|---|
| Pain | 72%*** | 87% |
| Bleeding | 78% | 83% |
| Nausea | 68%** | 85% |
| Vomiting | 67%* | 83% |
| Diarrhoea | 62% | 83% |
| Dizziness | 65%** | 84% |
P<0.05.
P<0.01.
P<0.001 comparing the frequency of satisfied women according to the presence of severe side effects, Fischer's exact test.
References
Abdel-Aziz E (
Bachelot A, Cludy L and Spira A (
Bartley J, Brown A, Elton R and Baird DT (
Beckman LJ and Harvey SM (
Belanger E, Melzack R and Lauzon P (
Cameron ST, Glasier AF, Logan J, Benton L and Baird DT (
Creinin MD and Shulman T (
Dahler-Eriksen K (
Gibb S, Donaldson C and Henshaw R (
Hakim-Elahi E, Tovell HM and Burnhill MS (
Harvey SM, Beckman LJ and Satre SJ (
Heisterberg L and Kringelbach M (
Henshaw RC, Naji SA, Russell IT and Templeton AA (
Honkanen H and von Hertzen H (
Howie FL, Henshaw RC, Naji SA, Russell IT and Templeton AA (
Kahn JG, Becker BJ, MacIsaa L, Amory JK, Neuhaus J, Olkin I and Creinin MD (
Lofgren, M (2000) Medical abortion, an alternative to surgical abortion?: Experience from 1000 cases.
Olschewski M, Schumacher M and Davis KB (
Rorbye C, Norgaard M and Nilas L (
Rorbye C, Norgaard M, Vestermark V and Nilas L (
Slade P, Heke S, Fletcher J and Stewart P (
UK Multicentre Study (
Westhoff C, Picardo L and Morrow E (
Winikoff B, Ellertson C, Elul B and Sivin I (
Wong SS, Bekker HL, Thornton JG and Gbolade BA (
Yuasa H, Kurita K and Westesson PL (
Author notes
1Department of Obstetrics and Gynecology, H:S Hvidovre Hospital, University of Copenhagen and 2Department of Obstetrics and Gynecology, H:S Frederiksberg Hospital, University of Copenhagen, Copenhagen, Denmark