Abstract
Objective:
The aim of this study was to assess overall inspiratory muscle activity during incremental exercise in obese men and healthy controls using the non-invasive, inspiratory muscle tension–time index (TT0.1). We studied 17 obese subjects (mean age±s.d.; 49±13 years) and 14 control subjects (42±16) during an incremental, maximal exercise test.
Methods:
Measurements included anthropometric parameters, spirometry, breathing patterns and inspiratory muscle activity. TT0.1 was calculated using the equation TT0.1=P0.1/PImax × TI/TTOT (where P0.1 is mouth occlusion pressure, PImax is maximal inspiratory pressure and TI/TTOT is the duty cycle).
Results:
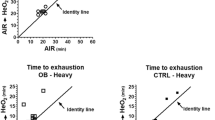
At same levels of maximal exercise (%Wmax) (20, 40, 60, 80, 100% Wmax), obese subjects showed higher P0.1 (P<0.001) and P0.1/PImax (P<0.001) values than controls. TT0.1 was thus higher in obese subjects for each workload increment and at maximal exercise (P<0.001).
Conclusions:
During exercise, patients with obesity show alterations in inspiratory muscle activity as a result of both reduced inspiratory strength (as measured by maximal inspiratory pressure) and increased ventilatory drive (as reflected by mouth occlusion pressure), which prone obese subject to respiratory muscle weakness. Our results suggest that impaired respiratory muscle activity could contribute to a decrease in exercise capacity. TT0.1 may be useful in our understanding concerning the benefits of endurance training.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Babb TG . Mechanical ventilatory constraints in aging, lung disease, and obesity: perspectives and brief review. Med Sci Sports Exerc 1999; 31: S12–S22.
DeLorey DS, Wyrick BL, Babb TG . Mild-to-moderate obesity: implications for respiratory mechanics at rest and during exercise in young men. Int J Obes (Lond) 2005; 29: 1039–1047.
Pankow W, Podszus T, Gutheil T, Penzel T, Peter J, Von Wichert P . Expiratory flow limitation and intrinsic positive end-expiratory pressure in obesity. J Appl Physiol 1998; 85: 1236–1243.
ATS/ERS. Statement on respiratory muscle testing. Am J Respir Crit Care Med 2002; 166: 518–624.
Bellemare F, Grassino A . Effect of pressure and timing of contraction on human diaphragm fatigue. J Appl Physiol 1982; 53: 1190–1195.
Ramonatxo M, Boulard P, Prefaut C . Validation of a noninvasive tension-time index of inspiratory muscles. J Appl Physiol 1995; 78: 646–653.
Gaultier C, Boule M, Tournier G, Girard F . Inspiratory force reserve of the respiratory muscles in children with chronic obstructive pulmonary disease. Am Rev Respir Dis 1985; 131: 811–815.
Chlif M, Keochkerian D, Mourlhon C, Choquet D, Ahmaidi S . Noninvasive assessment of the tension-time index of inspiratory muscles at rest in obese male subjects. Int J Obes (Lond) 2005; 29: 1478–1483.
Hayot M, Ramonatxo M, Matecki S, Milic-Emili J, Prefaut C . Noninvasive assessment of inspiratory muscle function during exercise. Am J Respir Crit Care Med 2000; 162: 2201–2207.
ATS/ERS. standardization of lung function testing: standardization of spirometry. Eur Respir J 2005; 26: 319–338.
Roca J, Burgos F, Sunyer J, Saez M, Chinn S, Anto JM et al. References values for forced spirometry. Group of the European Community Respiratory Health Survey. Eur Respir J 1998; 11: 1354–1362.
Black LF, Hyatt RE . Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis 1969; 99: 696–702.
Wasserman K, Hansen J, Sue D, Whipp B, Casaburi R . Principles of Exercise Testing and Interpretation. Lea & Febiger: Philadelphia, PA, 1994.
Borg G . Psychophysical basis of perceived exertion. Med Sci Sports Exerc 1982; 14: 377–381.
Hussain SN, Pardy RL, Dempsey JA . Mechanical impedance as determinant of inspiratory neural drive during exercise in humans. J Appl Physiol 1985; 59: 365–375.
Harik-Khan RI, Wise RA, Fozard JL . Determinants of maximal inspiratory pressure. The Baltimore Longitudinal Study of Aging. Am J Respir Crit Care Med 1998; 158: 1459–1464.
Grassino A, Goldman MD, Mead J, Sears TA . Mechanics of the human diaphragm during voluntary contraction: statics. J Appl Physiol 1978; 44: 829–839.
American Thoracic Society. Dyspnea. Mechanisms, assessment, and management: a consensus statement. Am J Respir Crit Care Med 1999; 159: 321–340.
Sahebjami H . Dyspnea in obese healthy men. Chest 1998; 114: 1373–1377.
Whitelaw WA, Derenne JP . Airway occlusion pressure. J Appl Physiol 1993; 74: 1475–1483.
Burki NK, Baker RW . Ventilatory regulation in eucapnic morbid obesity. Am Rev Respir Dis 1984; 129: 538–543.
Huang CH, Martin AD, Davenport PW . Effect of inspiratory muscle strength training on inspiratory motor drive and RREP early peak components. J Appl Physiol 2003; 94: 462–468.
Roussos C, Koutsoukou A . Respiratory failure. Eur Respir J Suppl 2003; 47: 3s–14s.
Leblanc P, Summers E, Inman MD, Jones NL, Campbell EJ, Killian KJ et al. Inspiratory muscles during exercise: a problem of supply and demand. J Appl Physiol 1988; 64: 2482–2489.
Wang LY, Cerny FJ . Ventilatory response to exercise in simulated obesity by chest loading. Med Sci Sports Exerc 2004; 36: 780–786.
Sampson MG, Grassino AE . Load compensation in obese patients during quiet tidal breathing. J Appl Physiol 1983; 55: 1269–1276.
Hsia CC . Cardiopulmonary limitations to exercise in restrictive lung disease. Med Sci Sports Exerc 1999; 31: S28–S32.
Kress JP, Pohlman AS, Alverdy J, Hall JB . The impact of morbid obesity on oxygen cost of breathing (VO(2RESP)) at rest. Am J Respir Crit Care Med 1999; 160: 883–886.
Jones NL, Killian KJ . Exercise limitation in health and disease. N Engl J Med 2000; 343: 632–641.
Acknowledgements
The authors thank the medical staff of the Department of Cardiac Rehabilitation of Corbie's Hospital for their technical assistance and the obese subjects from Nutritional and Physical Rehabilitation Department of Corbie's Hospital for their dedication to the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chlif, M., Keochkerian, D., Feki, Y. et al. Inspiratory muscle activity during incremental exercise in obese men. Int J Obes 31, 1456–1463 (2007). https://doi.org/10.1038/sj.ijo.0803546
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803546
Keywords
This article is cited by
-
Ventilatory Response at Rest and During Maximal Exercise Testing in Patients with Severe Obesity Before and After Sleeve Gastrectomy
Obesity Surgery (2021)
-
Air pollution inhalation during acute exercise is dependent of the body mass index and ventilation of young men
Environmental Science and Pollution Research (2020)
-
Obesity Surgery and Anesthesiology Risks: a Review of Key Concepts and Related Physiology
Obesity Surgery (2019)
-
Adiposity markers and lung function in smokers: a cross-sectional study in a Mediterranean population
BMC Pulmonary Medicine (2016)
-
Acute respiratory muscle unloading by normoxic helium–O2 breathing reduces the O2 cost of cycling and perceived exertion in obese adolescents
European Journal of Applied Physiology (2015)