Abstract
Purpose
Few interventions have been proven to improve outcomes in neurocritical care patients. It is unknown whether outcomes in Canada have changed over time. We performed a cohort study in Southern Alberta to determine whether survival and discharge disposition have improved.
Methods
Using prospectively collected data, we identified patients admitted to regional intensive care units (ICUs) over a more than 11-year period with traumatic brain injury (TBI), subarachnoid hemorrhage (SAH), intracerebral hemorrhage, anoxic encephalopathy, central nervous system infection, or status epilepticus. Four sequential time periods of 2.8 years were compared, as were periods before and after various practice modifications were introduced. Logistic regression was used to adjust for patient age, Glasgow Coma Scale score, and case mix.
Results
A total of 4,097 patients were assessed. The odds of death were lowest in the most recent time quartile (odds ratio [OR] 0.70, 95% confidence interval [CI] 0.56 to 0.88, P < 0.01). The odds of being discharged home without the need for support services increased over time (OR 1.45, 95% CI 1.38 to 1.85, P = 0.003). Improvements were not the same for all diagnostic subgroups. They were statistically significant for patients with TBI and SAH. Neurocritical care consultative services, evidence-based protocols, and clustering of patients within a multidisciplinary ICU were associated with improved outcomes. Length of stay in an ICU increased among hospital survivors (4.6 vs 3.8 days, P < 0.01).
Conclusions
Mortality and discharge disposition of neurocritical care patients in Southern Alberta have improved over time. Practice modifications in the region were associated with positive outcome trends. Longer ICU length of stay may imply that intensivists are increasingly delaying decisions about withdrawing life-sustaining interventions.
Résumé
Objectif
Très peu d’interventions sont reconnues comme améliorant le pronostic des patients en soins intensifs neurologiques. Nous ne savons pas si les pronostics ont changé au fil du temps au Canada. Nous avons réalisé une étude de cohorte dans le sud de l’Alberta afin de déterminer si la survie et la destination au congé de l’hôpital se sont améliorées.
Méthode
En nous fondant sur des données colligées de façon prospective, nous avons identifié les patients admis dans les unités de soins intensifs (USI) régionales sur une période de plus de 11 ans en raison de traumatisme cérébral, d’hémorragie sous-arachnoïdienne (HSA), d’hémorragie intracérébrale, d’encéphalopathie anoxique, d’infection du système nerveux central ou d’état de mal épileptique. Quatre périodes de temps séquentielles de 2,8 ans ont été comparées, ainsi que les périodes avant et après l’introduction de certaines modifications de la pratique. L’analyse par régression logistique a été utilisée pour prendre en compte l’âge des patients, leur score sur l’échelle de coma de Glasgow, et la clientèle.
Résultats
Au total, 4097 patients ont été évalués. La probabilité de décès était la plus faible dans le quartile temporel le plus récent (rapport de cotes [RC] 0,70, intervalle de confiance [IC] 95 % 0,56 à 0,88, P < 0,01). La probabilité de recevoir son congé sans avoir besoin de services de soutien a augmenté au fil du temps (RC 1,45, IC 95 % 1,38 à 1,85, P = 0,003). Les améliorations n’étaient pas les mêmes dans tous les sous-groupes diagnostiques. Ces améliorations étaient significatives d’un point de vue statistique pour les patients atteints de traumatisme cérébral et de HSA. Les services consultatifs en soins neurologiques, les protocoles fondés sur des données probantes et le regroupement des patients au sein d’une USI multidisciplinaire ont été associés à de meilleurs pronostics. La durée de séjour dans une USI a augmenté parmi les survivants à l’hôpital (4,6 vs. 3,8 jours, P < 0,01).
Conclusion
La mortalité et la destination au congé des patients en soins intensifs neurologiques se sont améliorées au fil du temps dans le sud de l’Alberta. Les modifications apportées à la pratique dans cette région ont été associées à des tendances vers de meilleurs pronostics. Une durée prolongée de séjour à l’USI pourrait signifier que les intensivistes retardent de plus en plus les décisions concernant le retrait des interventions de maintien de la vie.
Similar content being viewed by others
Approximately 15-20% of mechanically ventilated patients admitted to intensive care units (ICUs) have an admission diagnosis involving a neurocritical care condition.1 Compared with other critically ill populations, those with various forms of brain injury generally have worse outcomes. Apart from having a higher risk of death, those who survive are frequently left with various degrees of functional and cognitive limitations.2-8
Only a small number of specific interventions have been definitively demonstrated in large randomized controlled trials to improve outcomes in neurocritical care.9-14 Many of the treatments that are recommended in consensus guidelines and incorporated into protocols are, by necessity, based on low-quality evidence derived largely from observational studies.15-19 For example, over the past decade it has become common practice to prevent/treat aggressively even relatively mild derangements in core body temperature, blood glucose levels, and serum sodium and hemoglobin concentrations.20-23 With increasing use of electroencephalography, it has been recognized that many neurocritical care patients develop non-convulsive seizures, which most experts believe should be prevented or expeditiously diagnosed and treated.24 Care of patients is increasingly being individualized using multi-modal monitoring to adjust physiological goals, including intracranial pressure (ICP), cerebral perfusion pressure, and PCO2 or PO2 targets.25-27 Several observational studies have suggested that an organized, protocol-based approach with emphasis on the prevention of “secondary” neurological insults may be associated with improved recovery.28-34
Consistent with these developments, the care of neurocritical care patients in our region of Canada has evolved considerably over the past decade. There are few contemporary data assessing whether outcomes have changed. We performed a cohort study in Southern Alberta to assess whether hospital mortality and discharge disposition have improved. If they had, we wanted to explore whether certain practice modifications contributed and if the improvements were consistent across various diagnostic subgroups. Information concerning the natural history and prognosis of neurocritical care patients has important implications for bedside clinicians, health care administrators, and patients’ families.
Methods
The Research Ethics Board at the University of Calgary approved the study on June 28, 2012. The need for informed consent was waived, given that it was considered a quality assurance project. Explicit permission to publish results was provided.
The Alberta Health Services (Calgary Zone, previously Calgary Health Region) Department of Critical Care Medicine is responsible for administering critical care services at all hospitals for adults in Calgary. There are four closed ICUs located in three hospitals, including three “multi-system” and one post-cardiac surgical unit, all of which are staffed at all times by fellowship-trained critical care physicians. All critically ill patients with trauma, stroke, and/or neurosurgical conditions are cared for in an ICU at a single hospital, which serves as the only trauma and neurosurgical referral center for Southern Alberta. Some cardiac arrest patients, largely with acute coronary syndromes, are cared for in a coronary care unit. They are not included in this study.
Since 2001, information from all patients admitted to regional ICUs has been collected prospectively in a departmental database. At the time of ICU admission, attending critical care physicians are responsible for recording primary and secondary admission diagnoses using the Intensive Care National Audit & Research Centre coding method. This comprehensive system of recording admission diagnoses has been validated and demonstrated to have good inter-observer reliability.35 Each patient is given only one primary admission diagnosis but can be assigned multiple secondary diagnoses. The specific diagnostic codes used are listed in the Appendix. In addition, intensivists routinely document the admission Glasgow Coma Scale (GCS) score and relevant “chronic health points”, which in turn are combined with the most abnormal physiological data from the first 24 hr to calculate the Acute Physiology, Age, and Chronic Health Evaluation II (APACHE II) score.36 Computer specialists regularly monitor data entries and, if necessary, contact the attending physician to minimize the occurrence of missing data.
Using our database, we identified consecutive neurocritical care patients admitted to local ICUs between June 13, 2001 (start of the database) and July 28, 2012. We defined neurocritical care patients as having one of the following primary or secondary admission diagnoses, as determined by the admitting critical care physician: traumatic brain injury (TBI), subarachnoid hemorrhage (SAH), intracerebral hemorrhage (ICH), ischemic stroke, anoxic encephalopathy, central nervous system (CNS) infection, or status epilepticus. Patients with anoxic encephalopathy were included because by far the most common cause of death for survivors of out-of-hospital cardiac arrest is failure to awaken owing to severe neurological injury.37
The primary outcome of interest in this study was hospital mortality. Using information from the Alberta Health Services discharge abstract database, we were also able to determine whether patients had been discharged home (with or without support services), to another institution, or to a long-term nursing care facility. This information has been recorded prospectively since April 1, 2002 by each hospital’s Health Records Department. The discharge codes are listed in the Appendix. The two data sets—the first containing clinical data and the second discharge information—were linked using the patients’ unique medical record numbers. For the purposes of this study, we defined a “favourable” neurological recovery as one where the patient was discharged home without the need for support services.
To assess the association between the date of admission and eventual outcome, we divided the entire epoch into four shorter time periods with an equal number of days (n = 1,015 each): Period 1 was June 13, 2001 to March 25, 2004; Period 2 was March 26, 2004 to January 4, 2007; Period 3 was January 5, 2007 to October 16, 2009; Period 4 was October 17, 2009 to July 28, 2012).38 The rationale for dividing the data in this fashion was to minimize the impact of natural fluctuations in outcomes that might occur during shorter time intervals. We then used multivariable logistic regression models to adjust for patient age and the initial level of consciousness (assessed using the GCS score), both of which are known to be directly associated with mortality. These potential confounders were selected a priori because they are well known to be strongly associated with outcomes among neurocritical care patients with a variety of diagnoses.39-42 We also adjusted for diagnostic case mix (TBI vs other diagnoses), compared temporal trends between different diagnostic subgroups, and in a separate analysis considered time as a continuous variable (per 365-day block rather than for longer time periods). We also compared outcomes before and after certain developments in our region: availability of fellowship-trained neurocritical care specialists for consultation (September 2003); implementation of a temperature regulation protocol with availability of advanced cooling technology (endovascular catheters) (September 2004); mutual care rounds involving the ICU, neurocritical care, and neurosurgical services (July 2005); use of a comprehensive TBI management protocol (August 2008); and clustering of patients with neurocritical care diagnoses in a neurocritical care “pod” within a larger multidisciplinary unit (June 2010).
Because the APACHE II score includes age and GCS score as covariates, we calculated a modified score from which their contribution was subtracted. The APACHE II score is calculated based on the “worst” physiological values during the initial 24 hr in the ICU. It is generally considered to be a marker for baseline severity of illness. However, because the early resuscitation and care of critically ill patients can influence the 24-hr APACHE II score, it could also be viewed as an intermediate variable. Indeed, more effective early resuscitation could conceivably lead to a lower APACHE II score and, in turn, better outcomes. Given that statistical adjustment for an intermediate variable is inappropriate, we initially created our multivariable models without including the modified APACHE II score.43 However, we also performed a separate secondary analysis wherein we adjusted for it.
Statistical analysis was performed using SAS software (version 9.3; SAS Institute, Cary, NC, USA). Categorical variables were presented as proportions and compared using chi-square analysis. Continuous variables were presented as medians with the interquartile range and were compared using the Kruskall-Wallis test. Multivariable odds ratios (ORs) were presented with 95% confidence intervals (CIs). In cases where data were missing, the values were not replaced. A P value of < 0.05 indicated statistical significance.
Results
Patient characteristics
Between June 13, 2001 and July 28, 2012, a total of 4,097 patients admitted to regional ICUs had a primary or secondary neurocritical care diagnosis at admission. Patient characteristics are shown in Table 1. There was a somewhat lower proportion of patients with TBI and a higher proportion with status epilepticus during the most recent time period than during previous periods. Age and median GCS scores varied marginally among time periods but not in a consistent direction. APACHE II scores decreased slightly over time.
Patient outcomes
Hospital mortality data were available for all patients. The proportion of patients dying in hospital decreased significantly over time, from a maximum of 40% during the first time period to a minimum of 32% during the most recent epoch (Table 2; P = 0.001 for differences between the four time periods).
Discharge disposition data were available for 3,493 patients (85% overall, 91% since discharge abstracts were collected). The proportion of patients discharged home without the need for support services increased over time, from a minimum of 33% during the first period to 39%, 38%, and 40%, respectively, during subsequent time periods (Table 2; P < 0.001 for differences between time periods).
The median ICU stay among hospital survivors increased over time, ranging from 3.8 days for the first two time periods to 4.7 and 4.6 days, respectively, for the latter two time periods (Table 2; P < 0.01 for the difference between time periods). In contrast, among patients who died, the ICU stay did not change.
Multivariable analysis
With adjustment for patient age, initial GCS score, and diagnostic case mix (non-TBI vs TBI), there was a gradual reduction in the odds of hospital death from one time period to the next (Table 3). This association persisted with inclusion of the modified APACHE II score in the model as a potential confounder, rather than considering it to be an intermediate variable (OR 0.77, 95% CI 0.60 to 0.98, P = 0.03). A similar result was obtained when the admission date was assessed as a continuous variable (OR per year 0.96, 95% 0.94 to 0.99, P < 0.01).
As expected, patient age and the initial GCS score were powerful predictors of hospital mortality. Patients with diagnoses other than TBI had a higher mortality rate than patients with TBI.
A similar multivariable analysis, adjusting for the same covariates, was performed using “discharge home without the need for support services” as the outcome of interest (Table 3). The odds of being discharged home were significantly higher for the most recent time period than for the first time period. This was also true when the APACHE II score was included in the model (OR 1.40, 95% CI 1.09 to 1.79, P = 0.009). Using the admission date as a continuous variable, the OR (per year) was 1.05 with 95% CI 1.03 to 1.08 (P < 0.0001). When the analysis was restricted to patients who survived, the survivors during the last time period were significantly more likely to be discharged home without the need for support services (OR 1.41, 95% CI 1.08 to 1.85, P = 0.01).
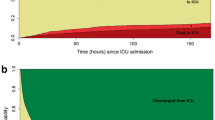
A pre-specified subgroup analysis was performed to assess the change in mortality over time (last time period vs first time period) according to the admitting diagnosis. Statistically significant reductions in mortality were observed for patients with TBI (OR 0.63, 95% CI 0.42 to 0.95, P = 0.03) and SAH (OR 0.49, 95% CI 0.25 to 0.95, P = 0.03). Comparable trends were observed for patients with anoxic brain injury, ICH, and status epilepticus but not for patients with ischemic stroke or CNS infection (Figure). When we repeated the multivariable analysis and included an interaction term for diagnostic category and time period of admission, there was evidence of a differential effect of time depending on the specific diagnosis (P < 0.0001).
Multivariable analysis assessing odds of hospital mortality during the most recent period compared with the initial time period based on the admitting diagnosis. Abbreviations: ICH = intracerebral hemorrhage; IS = ischemic stroke; SAH = subarachnoid hemorrhage; SE = status epilepticus; TBI = traumatic brain injury
Additional multivariable analyses were performed to assess mortality and discharge disposition before and after implementation of various changes in our region (Table 4). Each change that was introduced was associated with a favourable trend in subsequent outcomes.
Discussion
There has been a significant reduction in hospital mortality among neurocritical patients in Southern Alberta over the past 11 years. The proportion of patients discharged home without the need for support services (home care) has also increased. These changes persisted even with adjustment for variability in patient characteristics over time, including important prognostic factors such as age, initial level of consciousness (GCS score), diagnostic case mix (TBI vs other diagnoses), and severity of early physiological instability (APACHE II score). Improvements in outcomes were more obvious in some diagnostic subgroups than in others.
There are probably multiple reasons for improved outcomes in our region over time. During these 11 years, relevant changes have occurred, including hiring fellowship-trained neurointensivists to staff a consultative neurocritical care service; development of a temperature-regulation protocol, with increasing use of advanced technology (endovascular cooling catheters) aimed at achieving normothermia in most neurocritical care patients and therapeutic hypothermia in selected patients; collaborative morning rounds between ICU, neurocritical care, and neurosurgical services; adoption of a standardized regional protocol for the care of patients with severe TBI, with increasing use of multi-modal neurological monitoring (e.g., ICP, brain tissue oxygen tension, pressure reactivity, continuous electroencephalography, somatosensory evoked potentials, cerebral microdialysis) and a staged algorithm for treating intracranial hypertension; and clustering of neurocritical care patients (within a larger multi-system ICU) at the neurosurgical and trauma center (Foothills Medical Center) based on admission diagnosis. These changes in practice were temporally associated with reduced mortality and a greater proportion of patients discharged home without support (Table 4). Although we have provided specific dates in our analysis for when these changes were implemented, the principles underlying some of them were introduced more gradually. For example, many of the aspects of the local TBI management protocol had been embraced years before the protocol became an official document.
Over the past decade, there have been other gradual changes in practice that were not assessed in our analysis largely because there was no one specific time when they were implemented. Relevant examples might include increasing use of endovascular coil embolization to treat cerebral aneurysms; use of decompressive craniectomy to treat refractory intracranial hypertension and herniation syndromes; increasing availability of neurosurgical or neurological consultants with subspecialty interests; and more neurorehabilitation beds. Most of these changes in practice are not specifically supported by randomized controlled trials that have demonstrated their efficacy. Some practices, such as the use of hypothermia in TBI patients, decompressive craniectomy, and ICP monitoring, have been reported to lack efficacy at improving outcomes in preliminary clinical trials.44-46 Nevertheless, our findings are in agreement with multiple observational studies suggesting that the development of specialized neurocritical care units—usually supported by the presence of neurointensivists and utilizing evidence-based protocols—may contribute to improved patient outcomes.28
International studies involving neurocritical care patients have suggested that there is considerable variability in outcomes between countries and individual centers. Mortality rates have not consistently decreased among patients with TBI over the past two decades.47,48 Conflicting conclusions have been reached among patients with SAH and ICH, although trends have probably been favourable.49-53 There are relatively few corresponding Canadian data. A recent large national study involving more than 13,000 patients who had been resuscitated and hospitalized following cardiac arrest did not detect any improvements in survival rates over time.54 A study from Ontario using ICD-9 codes to identify hospitalized patients with TBI found no reduction in mortality between 1992 and 2001.55 Administrative databases have also been used to identify patients with hemorrhagic stroke from across Canada and to compare outcomes between 1982-1983 and 1991-1992. Statistically significant improvements in case-fatality rates were reported for patients with ICH but not SAH.56,57 In contrast to these findings, we have found substantial reductions in mortality rates for neurocritical care patients in Southern Alberta over the past decade.
Most deaths in critical care patients occur following the withdrawal of life-sustaining interventions.58,59 Opinions concerning the prognosis of neurocritical care patients vary among critical care practitioners. This variability may lead to significant differences in withdrawal-of-care practices,60-64 which in turn may explain some of the marked variability in outcomes that has been described, even within Canada.54,60 Some research has suggested that physicians may be generally more pessimistic about the prognosis of neurocritical care patients than is justified by their particular clinical characteristics.65 We found that the length of ICU stay among hospital survivors has increased over time, possibly indicating that local critical care physicians are delaying decisions related to withdrawal of life-sustaining interventions more often than previously. It is conceivable that this delay may have contributed to the reduction in mortality and the increasing proportion of patients who are discharged home.
Another observation based on our data was that 24-hr modified APACHE II scores (with the contribution of age and GCS removed) may have improved slightly over time, possibly implying that more recent patients receive more timely and complete resuscitation during the hours immediately following their neurological insult. Non-neurological organ dysfunction is an important predictor of outcomes in neurocritical care patients.66 Early physiological derangements are known to be associated with worse outcomes, and their timely correction could influence recovery.67-69 Consistent with this notion, one randomized controlled trial demonstrated that pre-hospital rapid sequence intubation (RSI) by paramedics increased the proportion of TBI patients with a favourable neurological recovery.14 Pre-hospital RSI was routine practice in Southern Alberta even before the time period assessed in this study. It is also possible that some of the improvements in outcomes that we observed in neurocritical care patients are attributable to advances in general critical care. However, another study assessing more than 25,000 consecutive patients admitted to ICUs in Calgary between 1999 and 2006 did not report any significant change in mortality.70
Our study is strengthened by the following factors: large cohort size (> 4,000 patients); long time period of interest (> 11 years); and prospective data collection by critical care physicians directly involved in patient care. Although not strictly a population-based study—we did not limit our cohort to Calgary residents—our study involved all consecutive patients with relevant diagnoses admitted to ICUs in Southern Alberta. Thus, our cohort is not subject to the referral biases of many single-center cohort studies and is a highly representative sample of neurocritical care patients within the population. The main limitation of our study is the lack of detailed long-term neurological outcome information. Discharge disposition data comprise an imperfect surrogate for neurological recovery. For example, patients who are transferred to another hospital may eventually be discharged home with a favourable recovery. In this study, such patients were characterized as having an unfavourable recovery. Conversely, some patients who are discharged home may remain severely disabled. The observation that an increasing number of neurocritical care patients in our region were eventually discharged home without the need for support services, however, suggests that the reduction in hospital mortality was not attributable simply to a greater proportion of survivors with a poor neurological recovery. Patients who survive in a profoundly disabled state are frequently unable to return home.
Conclusion
The proportion of critically ill neurological patients who survive and are discharged home has increased significantly in Southern Alberta over the past 11 years. These changes have been more pronounced in certain subgroups of patients, including those with TBI and SAH. Improved outcomes cannot necessarily be attributed to any one specific intervention. Our data suggest that contributing factors may include improvements in early resuscitation; availability of individuals with subspecialty expertise in neurocritical care; more attention to the prevention and expeditious treatment of factors that may contribute to secondary neurological injury; enhanced communication between critical care physicians and neuroscience specialists; increased use of standardized protocols; and changes in practices related to withdrawal of life-sustaining interventions. Implementation of some of these practices could potentially produce comparable improvements in outcomes in other regions. Further research is required to clarify which factors have the greatest impact on improving outcomes in neurocritical care patients and whether similar trends have occurred in other parts of Canada and the world.
References
Pelosi P, Ferguson ND, Frutos-Vivar F, et al. Management and outcome of mechanically ventilated neurologic patients. Crit Care Med 2011; 39: 1482-92.
Broessner G, Helbok R, Lackner P, et al. Survival and long-term functional outcome in 1,155 consecutive neurocritical care patients. Crit Care Med 2007; 35: 2025-30.
Gujjar AR, Deibert E, Manno EM, Duff S, Diringer MN. Mechanical ventilation for ischemic stroke and intracerebral hemorrhage: indications, timing, and outcome. Neurology 1998; 51: 447-51.
Christensen MC, Mayer S, Ferran JM. Quality of life after intracerebral hemorrhage: results of the Factor Seven for Acute Hemorrhagic Stroke (FAST) trial. Stroke 2009; 40: 1677-82.
Al-Khindi T, Macdonald RL, Schwiezer TA. Cognitive and functional outcome after aneurysmal subarachnoid hemorrhage. Stroke 2010; 41: e519-36.
Ruttan L, Martin K, Liu A, Colella B, Green RE. Long-term cognitive outcome in moderate to severe traumatic brain injury: a meta-analysis examining timed and untimed tests at 1 and 4.5 or more years after injury. Arch Phys Med Rehabil 2008; 89: S69-76.
Vaillancourt C. Stiell IG; Canadian Cardiovascular Outcomes Research Team. Cardiac arrest case and emergency medical services in Canada. Can J Cardiol 2004; 20: 1081-90.
Mateen FJ, Josephs KA, Trenerry MR, et al. Long-term cognitive outcomes following out-of-hospital cardiac arrest: a population-based study. Neurology 2011; 77: 1438-45.
Molyneux A, Kerr R, Stratton I, et al. International Subarachnoid Aneurysmal Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet 2002; 360: 1267-72.
Vahedi K, Hofmeijer J, Juettler E, et al. Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials. Lancet Neurol 2007; 6: 215-22.
Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med 2002; 346: 549-56.
Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med 2002; 346: 557-63.
De Gans J, van de Beek D. European Dexmethasone in Adulthood Bacterial Meningitis Study Investigators. Dexamethasone in adults with bacterial meningitis. N Engl J Med 2002; 347: 1549-56.
Bernard SA, Nguyen V, Cameron P, et al. Prehospital rapid sequence intubation improves functional outcome for patients with severe traumatic brain injury: a randomized controlled trial. Ann Surg 2010; 252: 959-65.
Diringer MN, Bleck TP. Claude Hemphioll J 3rd, et al. Critical care management of patients following aneurysmal subarachnoid hemorrhage: recommendations from the Neurocritical Care Society’s Multidisciplinary Consensus Conference. Neurocrit Care 2011; 15: 211-40.
Brain Trauma Foundation, American Association of Neurological Surgeons, Congress of Neurological Surgeons, et al. Guidelines for the management of severe traumatic brain injury. J Neurotrauma 2007; 24(Suppl): S1-106.
Morgenstern LB, Hemphill JC 3rd, Anderson C, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association / American Stroke Association. Stroke 2010; 41: 2108-29.
Brophy GM, Bell R, Claassen J, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care 2012; 17: 3-23.
Peberdy MA, Callaway CW, Neumar RW, et al. Part 9: post-cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S768-86.
Badjatia N. Hyperthermia and fever control in brain injury. Crit Care Med 2009; 37: S250-7.
Kramer AH, Roberts DJ, Zygun DA. Optimal glycemic control in neurocritical care patients: a systematic review and meta-analysis. Crit Care 2012; 22: R203.
Wright WL. Sodium and fluid management in acute brain injury. Curr Neurol Neurosci Rep 2012; 12: 466-73.
Kramer AH, Zygun DA. Anemia and red blood cell transfusion in neurocritical care. Crit Care 2009; 13: R89.
Kramer AH, Jette N, Pillay N, Federico P, Zygun DA. Epileptiform activity in neurocritical care patients. Can J Neurol Sci 2012; 39: 328-37.
Hemphill JC, Andrews P, De Georgia M. Multimodal monitoring and neurocritical care bioinformatics. Nat Rev Neurol 2011; 7: 451-60.
Stuart RM, Schmidt M, Kurtz P, et al. Intracranial multimodal monitoring for acute brain injury: a single institution review of current practices. Neurocrit Care 2010; 12: 188-98.
Tisdall MM, Smith M. Multimodal monitoring in traumatic brain injury: current status and future directions. Br J Anaesth 2007; 99: 61-7.
Kramer AH, Zygun DA. Do neurocritical care units save lives? Measuring the impact of specialized ICUs. Neurocrit Care 2011; 14: 329-33.
English SW, Turgeon AF, Owen E, Doucette S, Pagliarello G, McIntyre L. Protocol management of severe traumatic brain injury in intensive care units: a systematic review. Neurocrit Care 2013; 18: 131-42.
Diringer MN, Edwards DF. Admission to a neurologic/neurosurgical intensive care unit is associated with reduced mortality rate after intracerebral hemorrhage. Crit Care Med 2001; 29: 635-40.
Patel HC, Menon DK, Tebbs S, Hawker R, Hutchinson PJ, Kirkpatrick PJ. Specialist neurocritical care and outcome from head injury. Intensive Care Med 2002; 28: 547-53.
Elf K, Nilsson P, Enblad P. Outcome after traumatic brain injury improved by an organized secondary insult program and standardized neurointensive care. Crit Care Med 2002; 30: 2129-34.
Suarez JI, Zaidat OO, Suri MF, et al. Length of stay and mortality in neurocritically ill patients: impact of a specialized neurocritical care team. Crit Care Med 2004; 32: 2311-7.
Varelas PN, Conti MM, Spanaki MV, et al. The impact of a neurointensivist-lead team on a semiclosed neurosciences intensive care unit. Crit Care Med 2004; 32: 2191-8.
de Keizer NF, Bonsel GJ, Goldfad C, Rowan KM. The added value that increasing levels of diagnostic information provide in prognostic models to estimate hospital mortality for adult intensive care patients. Intensive Care Med 2000; 26: 577-84.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med 1985; 13: 818-29.
Laver S, Farrow C, Turner D, Nolan J. Mode of death after admission to an intensive care unit following cardiac arrest. Intensive Care Med 2004; 30: 2126-8.
Groenwold RH, Klungel OH, Altman DG, et al. Adjustment for continuous confounders: an example of how to prevent residual confounding. CMAJ 2013; 185: 401-6.
Hemphill JC 3rd, Farrant M, Neill TA Jr. Prospective validation of the ICH score for 12-month functional outcome. Neurology 2009; 73: 1088-94.
Rosengart AJ, Schultheiss KE, Tolentino J, Macdonald RL. Prognostic factors for outcome in patients with aneurysmal subarachnoid hemorrhage. Stroke 2007; 38: 2315-21.
Steyerberg EW, Mushkudiani N, Perel P, et al. Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. PLoS Med 2008; 5: e165.
van de Beek D, de Gans J, Spanjaard L, Weisfelt M, Reitsma JB, Vermeulen M. Clinical features and prognostic factors in adults with bacterial meningitis. N Engl J Med 2004; 351: 1849-59.
Braga LH, Farrokhyar F, Bhandari M. Confounding: what is it and how do we deal with it? Can J Surg 2012; 55: 132-8.
Clifton GL, Valadka A, Zygun D, et al. Very early hypothermia induction in patients with severe brain injury (the National Acute Brain Injury Study: Hypothermia II): a randomised trial. Lancet Neurol 2011; 10: 131-9.
Cooper DJ, Rosenfeld JV, Murray L, et al. Decompressive craniectomy in diffuse traumatic brain injury. N Engl J Med 2011; 364: 1493-502.
Chesnut RM, Temkin N, Carney N, et al. A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med 2012; 367: 2471-81.
Roozenbeek B, Maas AIR, Menon DK. Changing patterns in the epidemiology of traumatic brain injury. Nat Rev Neurol 2013; 9: 231-6.
Stein SC, Georgoff P, Meghan S, Mizra K, Sonnad SS. 150 years of treating severe traumatic brain injury: a systematic review of progress in mortality. J Neurotrauma 2010; 1343-53.
van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex and ethnic origin: a systematic review and meta-analysis. Lancet Neurol 2010; 9: 167-76.
Nieuwkamp DJ, Setz LE, Algra A, Linn FH, de Rooij NK, Rinkel GJ. Changes in case fatality of aneurysmal subarachnoid haemorrhage over time, according to age, sex, and region: a meta-analysis. Lancet Neurol 2009; 8: 635-42.
Feigin VL, Lawes CM, Bennett DA, Barker-Collo SI, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol 2009; 8: 355-69.
Sandvei MS, Mathiesen EB, Vatten LJ, et al. Incidence and mortality of aneurysmal subarachnoid hemorrhage in two Norwegian cohorts, 1984-2007. Neurology 2011; 77: 1833-9.
Lovelock CE, Rinkel GJ, Rothwell PM. Time trends in outcome of subarachnoid hemorrhage: population-based study and systematic review. Neurology 2010; 74: 1494-501.
Redpath C, Sambell C, Stiell I, et al. In-hospital mortality in 13,263 survivors of out-of-hospital cardiac arrest in Canada. Am Heart J 2010; 159: 577-83.e1.
Colantonio A, Croxford R, Farooq S, Laporte A, Coyte PC. Trends in hospitalization associated with traumatic brain injury in a publicly insured population, 1992-2002. J Trauma 2009; 66: 179-83.
Ostbye T, Levy AR, Mayo NE. Hospitalization and case-fatality rates for subarachnoid hemorrhage in Canada from 1982 through 1991. The Canadian Collaborative Study Group of Stroke Hospitalizations. Stroke 1997; 28: 793-8.
Mayo NE, Neville D, Kirkland S, et al. Hospitalization and case-fatality rates for stroke in Canada from 1982 through 1991. The Canadian Collaborative Study Group of Stroke Hospitalizations. Stroke 1996; 27: 1215-20.
Cook D, Rocker G, Marshall J, et al. Withdrawal of mechanical ventilation in anticipation of death in the intensive care unit. N Engl J Med 2003; 349: 1123-32.
Rocker G, Cook D, Sjokvist P, et al. Clinician predictions of intensive care unit mortality. Crit Care Med 2004; 32: 1149-54.
Turgeon AF, Lauzier F, Simard JF, et al. Mortality associated with withdrawal of life-sustaining therapy for patients with severe traumatic brain injury: a Canadian multicentre cohort study. CMAJ 2011; 183: 1581-8.
Cooper Z, Rivara FP, Wang J, MacKenzie EJ, Jurkovich GJ. Withdrawal of life-sustaining therapy in injured patients: variations between trauma centers and nontrauma centers. J Trauma 2009; 66: 1327-35.
Kelly AG, Hoskins KD, Holloway RG. Early stroke mortality, patient preferences, and the withdrawal of care bias. Neurology 2012; 79: 941-4.
Finley Caulfield A, Gabler L, Lansberg MG, et al. Outcome prediction in mechanically ventilated neurologic patients by junior neurointensivists. Neurology 2010; 74: 1096-101.
Racine E, Dion MJ, Wijman CA, Illes J, Lansberg MG. Profiles of neurological outcome prediction among intensivists. Neurocrit Care 2009; 11: 345-52.
Becker KJ, Baxter AB, Cohen WA, et al. Withdrawal of support in intracerebral hemorrhage may lead to self-fulfilling prophecies. Neurology 2001; 56: 766-72.
Zygun DA, Kortbeek JB, Fick GH, Laupland KB, Doig CJ. Non-neurologic organ dysfunction in severe traumatic brain injury. Crit Care Med 2005; 33: 654-60.
Murray GD, Butcher I, McHugh GS, et al. Multivariable prognostic analysis in traumatic brain injury: results from the IMPACT study. J Neurotrauma 2007; 24: 329-37.
Davis DP, Idris AH, Sise MJ, et al. Early ventilation and outcome in patients with moderate to severe traumatic brain injury. Crit Care Med 2006; 34: 1202-8.
Chesnut RM, Marshall LF, Klauber MR, et al. The role of secondary brain injury in determining outcome from severe head injury. J Trauma 1993; 34: 216-22.
Berthiaume LR, Peets AD, Schmidt U, et al. Time series analysis of use patterns for common invasive technologies in critically ill patients. J Crit Care 2009; 24: 471.e9-14.
Conflict of interest
This study was performed without any funding. The authors have no conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Andreas H. Kramer conceived and planned the study together with David A. Zygun, acquired the data, analyzed and interpreted the data, and wrote the manuscript. David A. Zygun conceived and planned the study together with Andreas H. Kramer, assisted with the analysis and interpretation of the data, and reviewed and approved the manuscript prior to submission.
Appendix
Appendix
-
I.
Intensive Care National Audit and Research Center (ICNARC) Diagnostic Codes for Neurocritical Care Conditions
-
Anoxic brain injury: “Anoxic or ischemic coma or encephalopathy”
-
Subarachnoid hemorrhage: “Subarachnoid bleeding”
-
CNS infection: “Meningitis”, “Encephalitis”, “Infected CSF shunt”, “Intracranial abscess”
-
Traumatic brain injury: “Subdural hematoma”, “Primary brain injury”, “Extradural hematoma”, “Non-accidental injury to brain”, “Non-accidental injury to brain”
-
Intracerebral hemorrhage: “Intracerebral bleeding”
-
Status epilepticus: “Status epilepticus or uncontrolled seizures”
-
Stroke: “Thrombo-occlusive disease of brain”, “Embolic brain lesions”, “Vasculitis of cerebral circulation”
-
Note: Patients were included in the cohort study if they had an admission primary or secondary diagnosis that included one of the above codes. Patients could only be assigned one primary admission diagnosis but could have multiple secondary diagnoses.
-
-
II.
Discharge Codes from Alberta Health Services Discharge Abstract Database
-
Transfer to another acute-care hospital
-
Transfer to a long-term care facility
-
Transfer to other care facility
-
Discharge to home with support services
-
Discharge home
-
Died, expired
-
Cadaver donor, admitted for organ/tissue removal
-
Rights and permissions
About this article
Cite this article
Kramer, A.H., Zygun, D.A. Declining mortality in neurocritical care patients: a cohort study in Southern Alberta over eleven years. Can J Anesth/J Can Anesth 60, 966–975 (2013). https://doi.org/10.1007/s12630-013-0001-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-013-0001-0