Abstract
Aim
Numerous reports in the 1990s pointed to a learning curve for laparoscopic cholecystectomy (LC), critical in achieving excellent outcomes. As LC is now standard therapy for acute cholecystitis (AC), we aimed to determine if surgeon volume is still vital to patient outcomes.
Methods
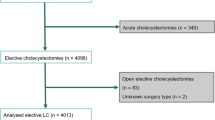
The Nationwide Inpatient Sample was used to query 80,149 emergent/urgent cholecystectomies performed for AC from 1999 to 2005 in 12 states with available surgeon/hospital identifiers. Volume groups were determined based on thirds of number of cholecystectomies performed per year for AC; two groups were created [low volume (LV): ≤15/year; high volume (HV): >15/year]. Primary endpoints were the rate of open conversion, bile duct injury (BDI), in-hospital mortality, and prolonged length of stay (LOS). Propensity scores were used to create a matched cohort analysis. Logistic regression models were created to further assess the effect of surgeon volume on primary endpoints.
Results
The number of cases performed by HV surgeons increased from 24% to 44% from 1999 to 2005. HV surgeons were more likely to perform LC, had fewer conversions, lower incidence of prolonged LOS, lower BDI, and lower in-hospital mortality. After matching the volume cohorts to create a case-controlled analysis, multivariate analysis confirmed that surgeon volume was an independent predictor of open conversion and prolonged LOS but not BDI and in-hospital mortality.
Conclusions
Increasing surgical volume remains associated with improved outcomes after surgery during emergent/urgent admission for AC with fewer open conversions and prolonged LOS. Our results suggest that referral to HV surgeons has improved outcomes after LC for AC.



Similar content being viewed by others
References
Angus DC, Shorr AF, White A, Dremsizov TT, Schmitz RJ, Kelley MA. Critical care delivery in the United States: distribution of services and compliance with Leapfrog recommendations. Crit Care Med. 2006;34:1016–1024.
Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002;288:2151–2162.
Hannan EL, Popp AJ, Feustel P, et al. Association of surgical specialty and processes of care with patient outcomes for carotid endarterectomy. Stroke. 2001;32:2890–2897.
Legorreta AP, Silber JH, Costantino GN, Kobylinski RW, Zatz SL. Increased cholecystectomy rate after the introduction of laparoscopic cholecystectomy. JAMA. 1993;270:1429–1432.
Rattner DW, Ferguson C, Warshaw AL. Factors associated with successful laparoscopic cholecystectomy for acute cholecystitis. Ann Surg. 1993;217:233–236.
Livingston EH, Rege RV. A nationwide study of conversion from laparoscopic to open cholecystectomy. Am J Surg. 2004;188:205–211.
Zacks SL, Sandler RS, Rutledge R, Brown RS Jr. A population-based cohort study comparing laparoscopic cholecystectomy and open cholecystectomy. Am J Gastroenterol. 2002;97:334–340.
The Southern Surgeons Club. A prospective analysis of 1518 laparoscopic cholecystectomies. N Engl J Med. 1991;324:1073–1078.
Csikesz NG, Tseng JF, Shah SA. Trends in surgical management for acute cholecystitis. Surgery. 2008;144:283–289.
Csikesz N, Ricciardi R, Tseng JF, Shah SA. Current status of surgical management of acute cholecystitis in the United States. World J Surg. 2008;32:2230–2236.
Mcphee JT, Hill JS, Whalen GF, et al. Perioperative mortality for pancreatectomy: a national perspective. Ann Surg. 2007;246:246–253.
Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117–2127.
Finlayson EV, Goodney PP, Birkmeyer JD. Hospital volume and operative mortality in cancer surgery: a national study. Arch Surg. 2003;138:721–725.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27.
Eppsteiner RW, Csikesz NG, Simons JP, Tseng JF, Shah SA. High volume and outcome after liver resection: surgeon or center? J Gastrointest Surg. 2008.
Cochran WG. The effectiveness of adjustment by subclassification in removing bias in observational studies. Biometrics. 1968;24:295–313.
Cook EF, Goldman L. Asymmetric stratification. An outline for an efficient method for controlling confounding in cohort studies. Am J Epidemiol. 1988;127:626–639.
Austin PC, Grootendorst P, Normand SL, Anderson GM. Conditioning on the propensity score can result in biased estimation of common measures of treatment effect: a Monte Carlo study. Stat Med. 2007;26:754–768.
Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127:757–763.
Everhart JE, Khare M, Hill M, Maurer KR. Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology. 1999;117:632–639.
Cowan JA Jr, Dimick JB, Thompson BG, Stanley JC, Upchurch GR Jr. Surgeon volume as an indicator of outcomes after carotid endarterectomy: an effect independent of specialty practice and hospital volume. J Am Coll Surg. 2002;195:814–821.
Harmon JW, Tang DG, Gordon TA, et al. Hospital volume can serve as a surrogate for surgeon volume for achieving excellent outcomes in colorectal resection. Ann Surg. 1999;230:404–411.
Birkmeyer JD, Sun Y, Goldfaden A, Birkmeyer NJ, Stukel TA. Volume and process of care in high-risk cancer surgery. Cancer. 2006;106:2476–2481.
Birkmeyer JD, Siewers AE, Marth NJ, Goodman DC. Regionalization of high-risk surgery and implications for patient travel times. JAMA. 2003;290:2703–2708.
Gordon TA, Bowman HM, Tielsch JM, Bass EB, Burleyson GP, Cameron JL. Statewide regionalization of pancreaticoduodenectomy and its effect on in-hospital mortality. Ann Surg. 1998;228:71–78.
Riall TS, Eschbach KA, Townsend CM Jr, Nealon WH, Freeman JL, Goodwin JS. Trends and disparities in regionalization of pancreatic resection. J Gastrointest Surg. 2007;11:1242–1251.
Mcmahon AJ, Fischbacher CM, Frame SH, Macleod MC. Impact of laparoscopic cholecystectomy: a population-based study. Lancet. 2000;356:1632–1637.
Ekeh AP, Monson B, Wozniak CJ, Armstrong M, Mccarthy MC. Management of acute appendicitis by an acute care surgery service: is operative intervention timely? J Am Coll Surg. 2008;207:43–48.
Green JM. When is faster better? Operative timing in acute care surgery. Curr Opin Crit Care. 2008;14:423–427.
Shah SA, Bromberg R, Coates A, Rempel E, Simunovic M, Gallinger S. Survival after liver resection for metastatic colorectal carcinoma in a large population. J Am Coll Surg. 2007;205:676–683.
Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–1137.
Acknowledgments
This article was supported by the American Society of Transplant Surgeons Faculty Development Award and Worcester Foundation for Biomedical Research (SAS).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Csikesz, N.G., Singla, A., Murphy, M.M. et al. Surgeon Volume Metrics in Laparoscopic Cholecystectomy. Dig Dis Sci 55, 2398–2405 (2010). https://doi.org/10.1007/s10620-009-1035-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-009-1035-6